Cannabis is used as an antiemetic and appetite stimulant for chemotherapy-associated nausea and for anorexia in HIV infection. The pathogenesis of paradoxical hyperemetic symptoms of CHS remain unclear, but several mechanisms have been proposed. The principle active cannabinoid in Cannabis is the highly lipophilic compound THC, which binds to cannabinoid type 1 (CB1) and type 2 (CB2) receptors in the CNS and other tissues. It is thought that the antiemetic and appetite-stimulating effects of Cannabis are mediated by CB1 receptor activation in the hypothalamus. Nausea and vomiting are thought to be mediated by CB1 receptor activation in the enteric nervous system, which causes slowed peristalsis, delayed gastric emptying, and splanchnic vasodilation.4,14
In sensitive persons, chronic heavy Cannabis use can cause THC to accumulate to a toxic level in fatty tissues, causing enteric receptor binding effects to override the CNS receptor-binding effects.4 This is supported by case studies describing severe vomiting with IV injection of crude marijuana extract.15 Nearly 100 different THC metabolites have been identified. The Cannabis plant contains more than 400 chemicals, with 60 cannabinoid structures, any of which could cause CHS in toxic concentrations.4,7 Among them, cannabidiol, a 5-HT1A partial agonist, was shown to cause vomiting at higher doses in animal studies.4,7
Mechanisms of action
Cannabis has been used for centuries, so it is unclear why CHS is only recently being recognized. It may be because of higher THC content through selective breeding of plants and a more selective use of female buds that contain more concentrated THC levels than leaves and stems.3 Alternately, CHS may be caused by exogenous substances, such as pesticides, additives, preservatives, or other chemicals used in marijuana preparation, although there is little evidence to support this.3
The mechanism of symptom relief with hot bathing also is unclear. Patients report consistent, global symptom improvement with hot bathing.3 Relief is rapid, transient, and temperature dependent.4 CB1 receptors are located near the thermoregulatory center of the hypothalamus. Increased body temperature with hot bathing may counteract the thermoregulatory dysregulation associated with Cannabis use.4,9 It has been proposed that splanchnic vasodilation might contribute to CHS symptoms. Thus, redistribution of blood from the gut to the skin with warm bathing causes a “cutaneous steal syndrome,” resulting in symptom relief.11
Diagnostic approach
Four key features should be present when making a diagnosis of CHS:
- heavy marijuana use
- recurrent episodes of severe nausea, vomiting, and abdominal cramping
- compulsive bathing for transient symptom relief
- resolution of symptoms with cessation of Cannabis use.2,4,8
Compulsive, hot bathing for symptom relief was described in 98% of all reported cases,3 and should be considered pathognomonic.2 CHS patients can present with other symptoms, including polydipsia, mild fever, weight loss, and orthostasis.3 Although lab studies usually are normal, mild leukocytosis, hypokalemia, hypochloremia, elevated salivary amylase, mild gastritis on esophagogastroduodenoscopy, and delayed gastric emptying have been described during acute episodes (Table 1).2-4,7,8
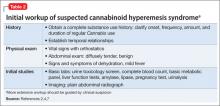
Diagnosis starts with a history and physical exam, followed by a basic workup geared towards ruling out other causes of acute nausea and vomiting.2,7 Establish temporal relationships between symptoms, Cannabis use (onset, frequency, amount, duration), and bathing behaviors. A positive urine toxicology screen supports a CHS diagnosis and can facilitate discussion of Cannabis use.2 If you suspect CHS, rule out potentially life-threatening causes of acute nausea, vomiting, and abdominal pain, such as intestinal obstruction or perforation, pancreaticobiliary disease, and pregnancy. The initial workup should include a CBC, basic metabolic panel, liver function tests, amylase, lipase, pregnancy test, urinalysis, urine toxicology screen, and abdominal radiographs (Table 2).2,4,7 The differential diagnosis of recurrent vomiting is broad and should be considered (Table 3).2,4,7,16 Further workup can proceed non-emergently, and should be prompted by clinical suspicion.2,7
Supportive treatment, education
Treatment of acute hyperemetic episodes in CHS primarily is supportive; address dehydration with IV fluids and electrolyte replenishment as needed.2,4,7 Standard antiemetics, including 5-HT3 receptor antagonists, D2 receptor antagonists, and H1 receptor antagonists, are largely ineffective.5,9 Although narcotics have been used to treat abdominal pain, use caution when prescribing because they can exacerbate nausea and vomiting.7 Case reports have described symptom relief with inpatient treatment with lorazepam12 and self-medication with alprazolam,4 but more evidence is needed. A recent case report described prompt resolution of symptoms with IV haloperidol.13 Treating gastritis symptoms with acid suppression therapy, such as a proton pump inhibitor, has been suggested.7 Symptoms abate during hospitalization regardless of treatment, marking the progression into the recovery phase with abstinence. There are no proven treatments for CHS, aside from cessation of Cannabis use. Treatment should focus on motivating your patient to stop using Cannabis.