Her early history is unremarkable. She did well in school. After earning a PhD at the University of Leipzig, she and her husband immigrated to Canada. Both are university professors. They never decided not to have children, but children hadn’t come. Her menstrual periods stopped 2 years before admission. The question about children is the only 1 that elicits emotion in Dr. I. When I ask about it, tears come to her eyes as she shakes her head.
Her husband reports that she has not been eating well and has, in the last year, started to drink more alcohol than usual—3 to 4 drinks of whiskey a night. She does not smoke cigarettes, and her health generally is good. She uses no medications. Her husband describes their marital relationship as very close, although it has become strained in recent weeks because of her unreasonable fears. He admits that their work is always stressful; competition is fierce, with more and more deadlines and less and less leisure time. The couple has few friends and no hobbies.
Late-onset psychosis symptoms
In late-onset psychosis (after age 45), men appear to suffer substantially milder symptoms and spend less time hospitalized than women.13 Women with late-onset schizophrenia have more severe positive symptoms than men and fewer negative symptoms.14,15 Overall, patients with late-onset schizophrenia have a lower prevalence of looseness of associations and negative symptoms than those with earlier onset.16,17
In addition, individuals with schizophrenia who become ill in middle age have been reported to:
• show better neuropsychological performance (particularly in learning and abstraction/cognitive flexibility) than those with early onset
• possibly have larger thalamic volumes
• respond to lower antipsychotic doses.18
Auditory and visual hallucinations frequently are observed in patients with comorbid late-onset schizophrenia and auditory and visual impairment.16 Palmer et al18 reported no difference in family history of schizophrenia between early and late onset, but this is controversial. Convert et al16 note that most studies reveal a lower lifetime risk of schizophrenia in first-degree relatives of patients with late-onset than early-onset schizophrenia.
CASE CONTINUED
Medical workup
Dr. I’s physical exam is unremarkable. Her thyroid is not enlarged; there are no breast lumps. On mental status exam, her mood is flat. She is preoccupied with fears of the Nazis. Routine blood tests show slight anemia; fasting glucose levels are within normal range.
I give Dr. I zopiclone, 7.5 mg, to help her sleep. The next day she keeps to herself, eats very little, and appears disinterested in her surroundings. Nursing staff report that she often seems frightened. Dr. I asks to use the ward phone to call Germany but is told that she cannot make long distance calls from that phone. This seems to disturb her.
Differential diagnosis
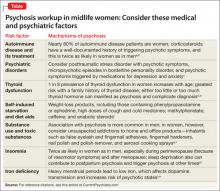
Sensory impairment, substance abuse, and metabolic changes have been implicated in the appearance of psychosis in later life. More specific to women than men, however, are medical and psychiatric precipitants. These include autoimmune disease (and its treatment) and psychiatric disorders, as well as thyroid dysfunction, self-induced starvation (anorexia nervosa) and diet aids, substance use and abuse, insomnia, and iron deficiency (Table).
Autoimmune disease and treatment. Nearly 80% of patients with autoimmune disease are women, and these disorders (as well as their treatment) can manifest as psychosis. Corticosteroids have a well-documented history of triggering psychotic symptoms, which are twice as likely in women than in men. The incidence of severe psychosis while taking oral prednisone ranges from 1.6% to 50% and averages 5.7%. The average daily dose of corticosteroids for patients who develop psychosis is 59.5 mg/d.
Corticosteroid creams absorbed through skin as well as inhaled and intranasal corticosteroids in their more potent formulations can have systemic effects, including psychosis. Nonsteroidal anti-inflammatory drugs such as ibuprofen also can trigger psychosis.19
Psychiatric disorders. Posttraumatic stress disorder with psychotic symptoms may overlap with categories such as psychogenic psychoses, hysterical psychoses, nonaffective remitting psychoses, acute brief psychoses, reactive psychoses, acute and transient psychoses, and bouffées délirantes (in France, the name for transient psychotic reactions).20 Consider these female-predominant conditions in the differential diagnosis, along with micropsychotic episodes in borderline personality disorder, in which the predominance of women is 3:1.
Medical treatment for depression and anxiety also can lead to psychotic symptoms through individual susceptibility to the action of specific drugs or through withdrawal effects.
Clinical assessment
Question all women presenting with psychosis about eating habits and diet pills, and check for hypokalemia and hypocalcemia to rule out starvation effects and reactions to stimulants. Also ask about inhalants, and examine for anemia and thyroid dysfunction. Consider all medications as having the potential to trigger psychotic symptoms.
A family history of illness is important, with a focus on autoimmune disorder and its treatment. A thorough psychiatric history is crucial and needs to include assessment of sleep, mood, and relationships with attachment figures. Do not assume illnesses of unknown cause (bipolar disorder or schizophrenia) until after a comprehensive search for precipitants of psychotic symptoms.