Neuralgia and neuroma secondary to iatrogenic saphenous nerve injury have been described in the setting of orthopedic surgical interventions using a medial parapatellar approach, and in vascular surgery procedures for harvest of the saphenous vein.1-3 However, postoperative neuropathic pain caused by saphenous neuroma in the setting of orthopedic trauma has not been described.
We present a case of symptomatic posttraumatic saphenous neuroma after a displaced and laterally angulated open distal one-third tibial fracture. This unreported cause of postinjury neuralgia is an important complication to address as other similar and more common conditions, such as peripheral neuropathy and complex regional pain syndrome (CRPS), can present in a similar manner. Reaching the correct diagnosis can be challenging for clinicians unfamiliar with this condition or its clinical presentation. The patient provided written informed consent for print and electronic publication of this case report.
Case Report
A 43-year-old woman presented to our practice 2 years after an open distal one-third metadiaphyseal fracture of the tibia with associated segmental fibular fracture (Gustilo-Anderson type II)4 after an automobile/bicycle accident. At the time of injury, she was noted to have a complex medial wound in the region of an open fracture at the junction of the middle and distal thirds of her tibial shaft. She underwent definitive treatment at an outside facility with initial irrigation and débridement and primary wound closure, followed by staged intramedullary nail fixation. Both soft-tissue and bony injuries healed within the expected time frame, and the patient was discharged from orthopedic care.
Approximately 1 year after her initial injury, the patient began to complain of progressive and persistent anteromedial knee pain as well as gradual-onset, medial-sided leg pain. The leg pain began at the level of her previous fracture site, at the distal one-third metadiaphyseal tibial junction, and radiated from the site of her previous medial open wound distally to the medial aspect of her foot. The pain was burning and tingling in nature, with associated hyperesthesia of the affected area. A diagnosis of CRPS was made, and the patient was prescribed a course of desensitization therapy, oral neuromodulating agents, and physical therapy. After 3 months’ therapy, she remained symptomatic and underwent removal of her proximal tibial interlocking screw fixation (Figure 1). When these measures failed to provide symptomatic relief, and having seen several therapists and physicians, including physiatrists, pain management specialists, and orthopedic surgeons, she presented to our clinic for consultation.
Diagnostic Assessment
On presentation, the patient’s surgical incisions were well healed. At the junction of the middle and distal thirds of the tibia, a 4-cm oblique scar was noted over the anteromedial border of the tibia, the site of her previous open fracture. She demonstrated decreased sensation along the length of this oblique scar, as well as in the distribution of the saphenous nerve distally. Further examination of the previously injured region revealed a positive Tinel sign over the course of the saphenous nerve, with radiating pain down the medial aspect of her leg, recreating her symptoms. She otherwise had full range of motion at the knee with mild tenderness to palpation at the medial joint line and patellar tendon. Her lower extremity motor examination, reflexes, and the remainder of her sensory examination were benign.
These findings were consistent with isolated saphenous neuralgia, and selective injection of the saphenous distribution over the injury site was performed. This injection provided immediate symptomatic relief, with the patient reporting preinjection and postinjection pain scores of 7/10 and 2/10, respectively. Because of the clinical improvement demonstrated with selective injection, surgical intervention with exploration and neurolysis of the saphenous nerve was recommended.
Therapeutic Intervention
The patient underwent surgical exploration of her saphenous nerve at the level of her original open fracture. This was done concurrently with a left-knee diagnostic arthroscopy and removal of her intramedullary tibial implant both to exclude intra-articular pathology (given her medial joint-line tenderness and the limitation of magnetic resonance imaging to diagnose meniscus tear in the presence of her tibial hardware) and to remove any potential hardware irritation in the setting of her anterior knee pain.5,6
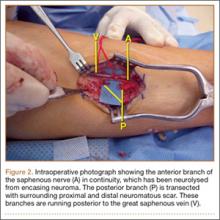
Preoperatively, the path of the saphenous nerve was marked using the saphenous vein as a guide. An incision overlying the presumed saphenous nerve course was made at the site of her previous open wound and clinical Tinel sign. The saphenous nerve was carefully dissected with loupe magnification, and the distal divisions of the anterior and posterior branches were identified. The anterior branch was found to be in continuity but encased in fibrotic neuroma. Selective neurolysis of this anterior branch was performed. The posterior branch was found to have been traumatically severed, with both the proximal and distal ends encased in neuromatous scar (Figure 2). Neurectomy of the posterior branch was performed and the severed proximal end of the nerve was buried into the adjacent medial gastrocnemius muscle beneath the fascia of the superficial posterior compartment.7-9