Adamantinomas are rare primary malignant bone tumors (less than 1% of all bone tumors) that arise most commonly in the tibia.1 There is a predilection for adult men aged 20 to 50 years, with rare occurrences in children. These tumors are malignant, highly invasive, and have significant metastatic potential.2 A rarely seen, benign variant, known as osteofibrous dysplasia–like adamantinoma, is described in the literature, with fewer than 135 cases reported.3-5 This variant predominantly has benign characteristics of an osteofibrous dysplasia lesion but has the potential to transform into an adamantinoma.6 Osteofibrous dysplasia–like adamantinoma has been observed to regress with age and is also referred to as a regressing adamantinoma or differentiated adamantinoma.7
We report an uncommon case of an osteofibrous dysplasia–like adamantinoma of the tibia in a 15-year-old girl. We decided to observe the tumor with regular 3- to 6-month follow-ups. Osteofibrous dysplasia–like adamantinoma in our patient has remained stable for 2 years and has an excellent prognosis.8 We report this case for its rarity, its short-term stability, and significant treatment implications due to its potential to regress or develop into a malignant form. The patient and the patient’s guardian provided written informed consent for print and electronic publication of this case report.
Case Report
A healthy 15-year-old girl was referred to our institution for evaluation of anterior left knee pain. She had sustained a fall while playing basketball 3 months earlier and had been having left knee pain since that time. She did not have any swelling, catching, or locking in her left knee. She denied any recent fever, chills, night sweats, weight loss, nausea, vomiting, or diarrhea. On physical examination, her gait was normal and no swelling, erythema, or tenderness was noticed around the left knee.
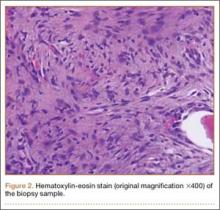
Plain radiographs revealed a heterogeneous lesion with sclerosis and thickening of the anteromedial cortex of the proximal left tibia (Figures 1A, 1B). A computed tomography (CT) scan of the abdomen, pelvis, and chest showed no osseous abnormalities. A whole-body bone scan showed activity in the anterior aspect of the left proximal tibia. No other areas of activity were noted. Magnetic resonance imaging of the left leg showed an elongated, multiloculated, enhancing mass arising from the anterolateral cortex and extending from the tibial tuberosity to the mid-diaphysis of the left tibia. Histologic examination of the CT-guided core needle biopsy specimen showed that the lesion was composed of dense fibrocollagenous tissue separating irregular bony trabeculae with osteoblastic and osteoclastic activity. There was no evidence of any atypical cells, necrosis, or significant mitotic activity. No epithelial cells were identified on hematoxylin-eosin (H&E) stain (Figure 2). However, immunohistochemical staining was positive for focal cytokeratin-positive epithelial cells (Figure 3). The lesion was diagnosed as an osteofibrous dysplasia–like adamantinoma on the basis of the radiographic and histologic findings. We elected nonoperative intervention given the benign nature of the lesion and its potential to regress. Given the possibility of sampling error and potential for progression, the patient was followed regularly at 3- to 6-month intervals over a 2-year period without disease progression.
Discussion
Osteofibrous dysplasia, osteofibrous dysplasia–like adamantinoma, and adamantinoma are rare fibro-osseous lesions that largely involve the midshaft of the tibia. Osteofibrous dysplasia accounts for 0.2% of primary bone tumors, whereas adamantinoma accounts for 0.1% to 0.5% of malignant bone tumors.9 Osteofibrous dysplasia is a benign lesion composed primarily of fibro-osseous tissue. Adamantinoma, however, is a slow-growing, low-grade, malignant biphasic tumor with intermingled epithelial and fibro-osseous components. It is an aggressive tumor that is locally invasive and can metastasize.2 Osteofibrous dysplasia–like adamantinoma (also known as differentiated or regressing adamantinoma) is a benign lesion like osteofibrous dysplasia but has features of both osteofibrous dysplasia and adamantinoma. Osteofibrous dysplasia–like adamantinoma may progress and become a malignant adamantinoma.6,10
The radiologic features of the 3 lesions are quite similar. It is not possible to distinguish between osteofibrous dysplasia and osteofibrous dysplasia–like adamantinoma based on imaging alone.9 Adamantinoma, being highly invasive, can be distinguished from osteofibrous dysplasia and osteofibrous dysplasia–like adamantinoma according to the extent of involvement of the medullary cavity seen on magnetic resonance imaging.9 Complete involvement of the medullary cavity is almost always seen in an adamantinoma. Involvement of the medullary cavity is minimal or absent in osteofibrous dysplasia and osteofibrous dysplasia–like adamantinoma lesions.
Tissue confirmation through biopsy is crucial for accurate diagnosis. A biopsy should always be performed on any suspicious lesion,3,6 and the fibro-osseous lesion should be treated as an adamantinoma if findings are equivocal. A biopsy also distinctly distinguishes these lesions from benign fibrous cortical defects, which have a similar radiographic appearance. While open biopsy is the gold standard, minimally invasive techniques such as core needle biopsy and fine needle biopsy are increasingly used.6 Because of the higher risk of misdiagnosis with minimally invasive techniques, radiographic confirmation is highly recommended.5