Tibial tubercle fractures are rare injuries accounting for less than 1% of all pediatric physeal injuries.1 The original classification scheme for such fractures was proposed by Watson-Jones.2 Initially modified by Ogden and colleagues,3 the classification system has had numerous additions and modifications as new patterns of injury have been identified.4-6 Patellar fractures are also rare in children, making up 1% of all pediatric fractures, with less than 2% of these occurring in skeletally immature children.7
We present a case of an unreported combined tibial tubercle avulsion fracture and patellar avulsion fracture in an adolescent boy. The patient and his guardian provided written informed consent for print and electronic publication of this case report.
Case Report
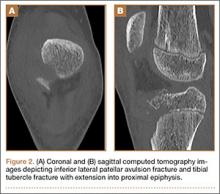
A 12-year-old boy presented to the emergency department with acute onset of right-knee pain and inability to ambulate after falling off a skateboard on the day of the injury. The patient was otherwise healthy and had no noteworthy medical or surgical history, including no prior fractures. On physical examination, he was noted to have a large right-knee effusion presumed to be hemarthrosis, and inability to perform a straight-leg raise against gravity. There were no neurologic deficits and his leg compartments were soft. Plain radiographs showed patella alta and numerous bony fragments believed to represent a complex tibial tubercle fracture. One bony fragment was identified closer to the patella, suggesting a possible concurrent patellar fracture (Figures 1A, 1B). A computed tomography (CT) scan further characterized both the tibial tubercle avulsion fracture and the lateral inferior pole patellar avulsion fracture (Figures 2A, 2B). The patient’s knee was immobilized, and he was admitted for soft-tissue rest and overnight observation to ensure that compartment syndrome did not develop.
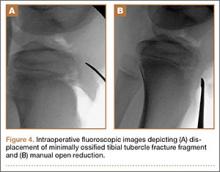
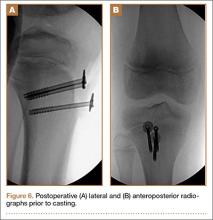
Five days after injury, open reduction and internal fixation were performed. After limb exsanguination and tourniquet insufflation, the fracture was visualized through a direct midline approach. The patient was found to have a Z-type injury pattern to the extensor mechanism: an inferior lateral patellar avulsion fracture, longitudinal splits of the patellar tendon, and 2 large, mainly cartilaginous tibial tubercle fracture fragments, 1 of which extended into the proximal tibial epiphysis (Ogden type III) (Figures 3A-3C). Under direct visualization, the tibial tubercle fragments were reduced and stabilized with 3 cannulated 3.5-mm titanium, partially threaded screws with washers. Smaller screws were used to prevent fragmentation of these mostly cartilaginous fragments. Anatomic reduction was ensured along the articular surface, visualized through an arthrotomy, as well as on the distal cortex (Figures 4A, 4B). The patellar avulsion fracture included a very small section of articular surface and the decision was made to preserve the fragment. Because the patellar fragment was too small for screw fixation, the fracture was secured with suture fixation through bone tunnels over a patellar bony bridge using size 2 Phantom Fiber suture (Tornier) (Figure 5). Vicryl was used to repair the longitudinal patellar tendon split as well as the capsular and paratenon traumatic tears. Layered closure was completed and intraoperative radiographs were obtained (Figures 6A, 6B) prior to placement of a cylinder cast in full extension. Postoperatively, the patient remained overnight for observation and physical therapy evaluation. He was encouraged to bear weight in his cylinder cast as tolerated with crutches to assist with ambulation.
Postoperatively, the patient was maintained in full extension in the cylinder cast for 4 weeks. After cast removal, the patient was placed in a range-of-motion brace locked in extension for ambulation. He started physical therapy and was allowed to perform prone active-knee flexion limited to 90º, with passive extension, for an additional 4 weeks. At 8 weeks, the patient was allowed full-knee motion both active and passive, and the brace was discontinued. At his 18-week follow-up appointment, the patient reported successful return to all his normal activities, including skateboarding, with no apparent limitation in motion or weight-bearing. Examination at that time demonstrated knee range of motion from 5º in hyperextension to 135º in flexion, with his left knee having 5º in hyperextension and 145º in flexion. The patient appeared to have no gait abnormalities, and radiographs showed healed fractures. Because of a concern that continued compression across his tibial physis could lead to greater risk of growth arrest, the decision was made to remove the implants when radiographs showed healing. The patient returned to surgery at 20 weeks for implant removal. At 6 weeks after implant removal, the patient had returned to full activity with no residual pain and full-knee flexion equal to the uninvolved left knee. He was able to perform a stable single-leg squat on his affected leg, and his single-leg hop for distance was the same as his uninvolved leg. He was allowed to return to full sports activity. The patient will be followed with serial radiographs at 4 months, 8 months, and 12 months to look for premature physeal arrest. If an arrest occurs, treatment will be dictated by the extent of the arrest and the potential to cause either limb-length difference or angular deformity.