The 2 cardinal properties of stem cells are the ability to self-renew and the ability to differentiate into distinctive end-stage cell types. The work of Caplan1 captured our early attention, with cells cultured from bone marrow differentiating into a number of different cell types of orthopedic interest. Our latest attention has been captured by the additional abilities of these cells to mobilize, monitor, and interact with their surrounding environment.2-4 In response to their environment, stem cells are able to release a broad spectrum of macromolecules with trophic, chemotactic, and immunomodulatory potential, which allows them to participate in injury response, tissue healing, and tissue regeneration.4 These cells are innate to the body’s monitoring, maintenance, repair, and stress response systems.2,4-11 Basic science and animal studies have illustrated the potential of cells with stem potential regardless of their environment/source of harvest.
Where Can We Get Stem Cells?
Cells with stem properties are present in many environmental niches, including the bone marrow, peripheral circulatory system, adipose tissue, synovial tissue, muscle tissue, and tendon tissue.12-15 A number of cell types with stem properties populate the bone marrow niche, including hematopoietic stem/progenitor cells (HSPC), perivascular stromal cells (PSC), endothelial stem cells (ESC), and immature cells with qualities like embryonal stem cells termed very small embryonal-like stem cells (VESL).12,15-19 All of these cells have stem properties and have been shown to differentiate to tissues of orthopedic interest.The interplay, interaction, and potential of these cell types is complex and incompletely understood.12,15-19 When bone marrow is aspirated for culturing purposes, it is unclear which cell line produces the plastic-adherent multipotent cells grown in culture, which are often referred to as mesenchymal stem cells (MSCs). Researches propose that HSPC and/or VESL circulate peripherally in small numbers but leave the bone marrow in certain mobilization instances and are important for the monitoring and maintenance of the majority of tissues in our bodies.5,16 Current clinical utilization of these cell types by the orthopedic community primarily utilizes point-of-care bone marrow aspiration and concentration, while the hematology oncology community mobilizes cells from the bone marrow to the blood stream with pharmaceutical agents and harvests cells via apheresis. Bone marrow aspiration produces variable numbers of stem cells, with studies ranging from 1 stem cell per mL of tissue collected to 300,000 stem cells per mL of tissue collected.20Mobilization and apheresis can produce large volumes of peripheral blood-derived cells with 600,000 HSPC per mL and 2.32 million PSC per mL of tissue collected.21
In adipose tissue, cells adherent to the abluminal side of blood vessels known as pericytes also carry stem qualities. Aspiration and processing of adipose tissue can access these stem cells, producing a product often referred to as stromal vascular fraction (SVF). Processing of lipoaspirate to create stromal vascular fraction requires mechanical or enzymatic processing. This also produces variable numbers of stem cells, with quantitative studies ranging from 5000 to 1.5 million stem cells per mL of tissue collected.20 Similar to adipose-derived stem cells, synovial-derived and muscle-derived stem cells also require mechanical or enzymatic processing. For applications where it is believed that a large number of cells is necessary, investigators often utilize culturing techniques for all sources with the exception of mobilization and apheresis harvest. As clinicians, 3 challenges have proven more important than which cell type to utilize: 1) patient-care logistics regarding collection and application; 2) the undefined dose-response curve regarding stem cell treatments; and 3) evolving government/community regulation.
Regulation of Stem Cell Therapies
The regulation of stem cell technologies is a double-edged sword for development. While loose regulation encourages clinical application and experimentation, patient safety and efficacy concerns are raised, and a technology’s worth is not proven before clinical application. Tight regulation temporarily hampers progress, yet ensures the proof of safety and efficacy prior to widespread implementation. Within the United States, the Food and Drug Administration (FDA) has tightened regulation, established precedent, and intervened in the ability of clinicians to utilize stem cell therapies in humans, through “warning letters,” “untitled letters,” and industry guidance documents.22-30
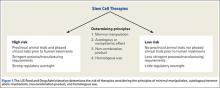
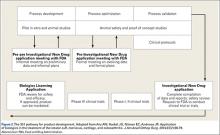
The FDA categorizes stem cell therapies as human cells, tissues, and cellular- and tissue-based products (HCT/Ps). Section 361 of the Public Health Safety (PHS) Act established and outlined the authority of the FDA to regulate low-risk HCT/Ps in order to prevent the introduction, transmission, and spread of communicable disease. Section 361 provided standards for safety without requiring preclinical development. The FDA established 4 principles to determine the risk of HCT/Ps: the extent of manipulation involved in manufacture, the metabolic activity/autologous nature of the product, whether the product represents a tissue combined with another product, and whether the product is utilized in a fashion homologous with its original function (Figure 1). If a product/therapy meets requirements around all 4 of these principles, then it is deemed a low-risk product and regulated under Section 361 alone. If a product/therapy does not meet requirements around all 4 of these principles, then the FDA regulates the product/therapy under additional codes including Section 351 of the PHS Act. Section 351 outlines a developmental process including preclinical animal trials, phased clinical study, and premarket review by the FDA prior to offering the product/treatment in clinical practice. The developmental process requires investigators and/or industry developers to initiate an Investigational New Drug (IND) program whose end goal is to present data from all developmental study and obtain a Biologic License Application (BLA) approval to market the product.22-23 To establish safety and efficacy, the traditional IND program involves a preclinical animal study, a small pilot human study (Phase I), a small initial randomized controlled trial (Phase II), followed by a large multicenter randomized controlled trial (Phase III) (Figure 2). The FDA has recognized little to no stem cell treatments as products regulated by Section 361 alone. Additionally, the FDA has established precedent regarding allograft stem cells, cells obtained from fat harvest, amniotic/placental products, and cultured cells, suggesting that these products are not low risk and require an IND pathway outlined in Section 351.24-30