This patient had undergone functional complete medial meniscectomy and had significant medial compartment pain, varus alignment, and minimal medial joint-space narrowing (assumed grossly intact cartilage about plateau and condyle), plus patellofemoral pain and crepitance with a large high-grade posttraumatic patellar chondral lesion with normal patellofemoral alignment. He also had an isolated failed ACL graft from prior ACL reconstruction. The previous hardware placement was analyzed, and it was determined that the femoral interference screw could be left in place and that the tibial interference screw most likely would be removed. The mechanical axis determined from the bilateral long-leg standing images dictated a need for proximal OWMTO for correction up to 8° to allow the axis to cross the center of the knee. The 8° correction is the measured correction needed to move the axis from its pass through the medial compartment to a more balanced position across the middle of the knee.
The overall plan encompassed major concomitant corrective and restorative surgery: tibial osteotomy, medial MAT, revision ACL reconstruction, and fresh mega-patellar OCA. Once the frozen meniscus and eventually the fresh patella (both matched for size) were obtained, arrangements for the patient’s trip for the complex surgery were finalized.
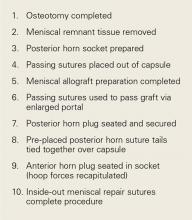
Surgery was started with brief arthroscopic evaluation to confirm the overall appropriateness of the planned procedure and to determine if any other minor deficiencies would warrant operative intervention. Once confirmed, the restoration proceeded as planned. The OWMTO was performed with a PEEK (polyetheretherketone) wedge implant (iBalance; Arthrex) followed by arthroscopic preparation for medial MAT with removal of any meniscal remnants and placement of passing sutures (Figure 2A).
The meniscus was delivered across the compartment through an enlarged medial portal. The posterior horn bone plug was secured in the retrosocket with sutures tied off to an anterior tibial cortical 2-hole button (Figure 2B). The body of the posterior third of the meniscus was secured to the posterior capsule by tying the 2 previously placed vertical sutures to each other over the intervening capsule. The anterior horn bone plug (10 mm in diameter × 7 mm thick) was then secured within a 10-mm socket drilled antegrade to a depth of 10 mm with a SwiveLock anchor (Arthrex) for interference bony fixation and recapitulation of the normal hoop stresses. Inside-out sutures were placed to secure the capsule to the meniscus and thereby prevent iatrogenic meniscal extrusion. A standard all-inside allograft revision ACL reconstruction was performed with an 11-mm FlipCutter and guide system (Arthrex) to make the femoral and tibial retrosockets. Passing sutures were used to deploy the ACL graft construct, which was fashioned into a quadruple-stranded GraftLink construct (Arthrex) from a 28-mm allograft peroneus longus tendon (Figure 3).When the arthroscopic portion of the surgery was finished, a medial parapatellar arthrotomy was made to allow the patella to be inverted and complete fresh mega-patellar OCA placement (Figure 4).
A drill guide system was used to prepare the host patella with the largest contained circular socket (35 mm) with a 1-mm to 2-mm cortical margin to a marginal bony depth and an 8- to 10-mm central bony depth. The donor patella was then prepared on the graft preparation guide to allow a mega-patellar osteochondral plug to be press-fit into the recipient socket after thorough pulse lavaging of the bony portion of the graft to negate as much of the marrow cellular elements as possible (Figure 5). After appropriate tracking was confirmed, the arthrotomy and skin incision were closed.The knee was placed in a ROM brace locked in full extension. The patient was able to do straight-leg raises and calf pumps in the recovery room and was discharged home with a saphenous nerve block and an iPACK (Interspace between the Popliteal Artery and the Capsule of the posterior Knee) nerve block in place. Home-based therapy was started immediately. After the patient’s first postoperative visit, formal therapy (discussed earlier) was initiated (Figure 6).
Toe-touch weight-bearing with the brace locked in extension and ROM limited to 0° to 90° were maintained until 6 weeks, when full weight-bearing and full ROM were allowed. The rehabilitation course was uneventful. The patient continued on active duty and completed his military service, retiring 3 years later with 20 years of service.Discussion
All-inside GraftLink ACL reconstruction with cortical suspensory fixation appears well suited to combined medial and lateral MAT and/or cartilage restoration—whether it be large fresh OCA combined with medial MAT (as in this patient’s case) or another form of cartilage restoration. Arthroscopic MAT with anatomically fashioned and placed bone plugs minimizes the morbidity within the notch footprints and allows for discrete revision socket formation for both femoral and tibial ACL graft placement. In this case, preparation for the medial MAT and ACL sockets was followed by MAT/ACL construct implantation and secure fixation. The arthrotomy was thereby minimized and placed to allow for efficient mega-patellar OCA graft placement.
Over the past decade, I have performed similar concomitant procedures using the same surgical principles that allow for efficient and reproducible complex knee restoration (Figure 7).
Common examples are multiligamentous reconstructions (ACL–posterior cruciate ligament–posterolateral corner, ACL–posterior cruciate ligament–medial collateral ligament, ACL–anterolateral ligament, and ACL–medial patellofemoral ligament) combined with concomitant meniscus and cartilage restoration and various osteotomies.Although use of an algorithm for the management of complex knee restorations is not universally feasible, I offer guidelines for complex knee injuries:
- At each decision point, determine whether the knee and the patient can withstand the planned surgical intervention.
- After deciding to proceed with knee restoration, list the meniscus, cartilage, and ligament injuries that must be addressed.
- Determine which repairs (meniscus, cartilage, ligament) are warranted. Repairs generally are best performed within a period of 7 to 14 days.
- Determine which ligament injuries warrant reconstruction. Allograft tissue typically is used for multiligament reconstruction.
- Rank-order the ligament reconstruction requirements. It is fine to proceed with all of the reconstructions if the case is moving smoothly, if there are no developing tourniquet-time issues, and if the soft-tissue envelope is responding as expected.
- Consider autograft and/or allograft tissue needs for concomitant or staged meniscus and cartilage restoration options/requirements.
Am J Orthop. 2017;46(4):170-175, 202. Copyright Frontline Medical Communications Inc. 2017. All rights reserved.