Take-Home Points
- Novel synovial markers and PCR have the potential to improve the detection of PJIs.
- 10Difficult-to-detect infections of prosthetic joints pose a diagnostic problem to surgeons and can lead to suboptimal outcomes.
- AD is a highly sensitive and specific synovial fluid marker for detecting PJIs.
- AD has shown promising results in detecting low virulence organisms.
- Studies are needed to determine how to best incorporate novel synovial markers and PCR to current diagnostic criteria in order to improve diagnostic accuracy.
Approximately 7 million Americans are living with a hip or knee replacement.1 According to projections, primary hip arthroplasties will increase by 174% and knee arthroplasties by 673% by 2030. Revision arthroplasties are projected to increase by 137% for hips and 601% for knees during the same time period.2 Infection and aseptic loosening are the most common causes of implant failure.3 The literature shows that infection is the most common cause of failure within 2 years after surgery and that aseptic loosening is the most common cause for late revision.3
Recent studies suggest that prosthetic joint infection (PJI) may be underreported because of difficulty making a diagnosis and that cases of aseptic loosening may in fact be attributable to infections with low-virulence organisms.2,3 These findings have led to new efforts to develop uniform criteria for diagnosing PJIs. In 2011, the Musculoskeletal Infection Society (MSIS) offered a new definition for PJI diagnosis, based on clinical and laboratory criteria, to increase the accuracy of PJI diagnosis.4 The MSIS committee acknowledged that PJI may be present even if these criteria are not met, particularly in the case of low-virulence organisms, as patients may not present with clinical signs of infection and may have normal inflammatory markers and joint aspirates. Reports of PJI cases misdiagnosed as aseptic loosening suggest that current screening and diagnostic tools are not sensitive enough to detect all infections and that PJI is likely underdiagnosed.
According to MSIS criteria, the diagnosis of PJI can be made when there is a sinus tract communicating with the prosthesis, when a pathogen is isolated by culture from 2 or more separate tissue or fluid samples obtained from the affected prosthetic joint, or when 4 of 6 criteria are met. The 6 criteria are (1) elevated serum erythrocyte sedimentation rate (ESR) (>30 mm/hour) and elevated C-reactive protein (CRP) level (>10 mg/L); (2) elevated synovial white blood cell (WBC) count (1100-4000 cells/μL); (3) elevated synovial polymorphonuclear leukocytes (>64%); (4) purulence in affected joint; (5) isolation of a microorganism in a culture of periprosthetic tissue or fluid; and (6) more than 5 neutrophils per high-power field in 5 high-power fields observed.
In this review article, we discuss recently developed novel synovial biomarkers and polymerase chain reaction (PCR) technologies that may help increase the sensitivity and specificity of diagnostic guidelines for PJI.
Methods
Using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses), we performed a systematic review of specific synovial fluid markers and PCR used in PJI diagnosis. In May 2016, we searched the PubMed database for these criteria: ((((((PCR[Text Word]) OR IL-6[Text Word]) OR leukocyte esterase[Text Word]) OR alpha defensin[Text Word]) AND ((“infection/diagnosis”[MeSH Terms] OR “infection/surgery”[MeSH Terms])))) AND (prosthetic joint infection[MeSH Terms] OR periprosthetic joint infection[MeSH Terms]).
We included patients who had undergone total hip, knee, or shoulder arthroplasty (THA, TKA, TSA). Index tests were PCR and the synovial fluid markers α-defensin (AD), interleukin 6 (IL-6), and leukocyte esterase (LE). Reference tests included joint fluid/serum analysis or tissue analysis (ESR/CRP level, cell count, culture, frozen section), which defined the MSIS criteria for PJI. Primary outcomes of interest were sensitivity and specificity, and secondary outcomes of interest included positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (+LR), and negative likelihood ratio (–LR). Randomized controlled trials and controlled cohort studies in humans published within the past 10 years were included.
Results
Our full-text review yielded 15 papers that met our study inclusion criteria (Figure 1).
α-Defensin
One of the novel synovial biomarkers that has shown significant promise in diagnosing PJIs, even with difficult-to-detect organisms, is AD.
Frangiamore and colleagues5 conducted a prospective study comparing patients with painful TSAs that required revision (n = 33). Patients were grouped based on objective clinical, laboratory, and histologic criteria of infection, which included preoperative clinical signs (swelling, sinus track, redness, drainage), elevated serum ESR or CRP, intraoperative gross findings (purulence, necrosis) and positive intraoperative frozen section. Synovial fluid aspiration was obtained preoperatively or intraoperatively. Of the 33 patients, 11 patients met the authors criteria for suspected PJI prior to final intraoperative culture results; 22 patients did not. Of the samples taken intraoperatively, Propionibacterium acnes was the most commonly isolated organism (9 cases), followed by coagulase-negative Staphylococcus (4 cases). AD demonstrated a sensitivity of 63%, specificity of 95%, +LR ratio of 12.1, and –LR ratio of 0.38. AD showed a strong association with growth of P acnes in the infected group (median signal-to-cutoff ratio, 4.45) compared with the noninfected group (median signal-to-cutoff ratio, 1.33) as well as strong associations with frozen section histology. Frangiamore and colleagues5 concluded that the use of AD in diagnosing PJIs with difficult-to-detect organisms was promising.AD has shown even more impressive results as a biomarker for PJI in the hip and knee, where infection with low virulence organism is less common. In 2014, Deirmengian and colleagues6 conducted a prospective clinical study of 149 patients who underwent revision THA or TKA for aseptic loosening (n = 112) or PJI (n = 37) as defined by MSIS criteria. Aseptic loosening was diagnosed when there was no identifiable reason for pain, and MSIS criteria were not met. Synovial fluid aspirates were collected before or during surgery. AD correctly identified 143 of the 149 patients with confirmed infection with sensitivity of 97.3% (95% confidence interval [CI], 85.8%-99.6%) and specificity of 95.5% (95% CI, 89.9%-98.5%). Similarly, Bingham and colleagues7 conducted a retrospective clinical study of 61 assays done on 57 patients who underwent revision arthroplasty for PJI as defined by MSIS criteria. Synovial fluid aspirates were collected before or during surgery. AD correctly identified all 19 PJIs with sensitivity of 100% (95% CI, 79%-100%) and specificity of 95% (95% CI, 83%-99%). Sensitivity and specificity of the AD assay more accurately predicted infection than synovial cell count or serum ESR/CRP level did.
These results are supported by another prospective study by Deirmengian and colleagues8 differentiating aseptic failures and PJIs in THA or TKA. The sensitivity and specificity of AD in diagnosing PJI were 100% (95% CI, 85.05%-100%).
Synovial fluid was collected from 46 patients before and during surgery: 23 with PJI and 23 with aseptic failure as defined by MSIS criteria. All patients were tested for AD or LE. Of the 23 PJI cases, 18 were associated with a positive culture, with the most common organism being Staphylococcus epidermidis (n = 6). AD correctly diagnosed 100% of PJIs, whereas LE correctly diagnosed only 78%; the difference was statistically significant (P < 0.001).In a prospective study of 102 patients who underwent revision THA or TKA secondary to aseptic loosening or PJI, Frangiamore and colleagues9 also demonstrated the value of AD as a diagnostic for PJI in primary and revision hip and knee arthroplasty.
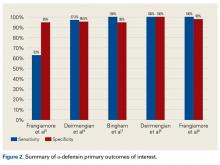
Based on MSIS criteria, 54 cases were classified as non-infected first-stage revision, 24 as infected first-stage revision, 35 as non-infected second-stage revision, and 3 as infected second-stage revision. For patients with first-stage revision THA or TKA, AD had sensitivity of 100% (95% CI, 86%-100%), specificity of 98% (95% CI, 90%-100%), PPV of 96% (95% CI, 80%-99%), and NPV of 100% (95% CI, 93%-100%). +LR was 54 (95% CI, 8-376), and –LR was 0. When combining all patients, AD outperformed serum ESR and CRP and synovial cell count as a biomarker for predicting PJI.Table 1 and Figure 2 provide a concise review of the findings of each study.
Interleukin 6
Another synovial fluid biomarker that has shown promise in PJI diagnosis is IL-6. In 2015, Frangiamore and colleagues10 conducted a prospective clinical study of 32 patients who underwent revision TSA. Synovial fluid aspiration was obtained before or during surgery. MSIS criteria were used to establish the diagnosis of PJI. IL-6 had sensitivity of 87% and specificity of 90%, with +LR of 8.45 and –LR of 0.15 in predicting PJI. Synovial fluid IL-6 had strong associations with frozen section histology and growth of P acnes. Frangiamore and colleagues10 recommended an ideal IL-6 cutoff of 359.1 pg/mL and reported that, though not as accurate as AD, synovial fluid IL-6 levels can help predict positive cultures in patients who undergo revision TSA.
Lenski and Scherer11 conducted another retrospective clinical study of the diagnostic value of IL-6 in PJI.
Revision total joint arthroplasty (TJA) was performed for aseptic loosening (38 patients) or PJI (31 patients) based on criteria modeled after MSIS criteria. All joints were aspirated for synovial fluid IL-6, synovial fluid lactate dehydrogenase, synovial fluid glucose, synovial fluid lactate, synovial fluid WBCs, and serum CRP. IL-6 had sensitivity of 90.9%, specificity of 94.7%, +LR of 17.27, and –LR of 0.10. An optimal IL-6 cutoff value of 30,750 pg/mL was determined.Randau and colleagues12 conducted a prospective clinical study of 120 patients who presented with painful THA or TKA and underwent revision for PJI, aseptic failure, or aseptic revision without signs of infection or loosening. Synovial fluid aspirate was collected before or during surgery.
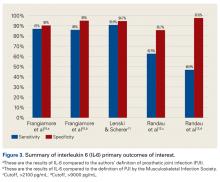
PJI was diagnosed with the modified MSIS criteria. IL-6 sensitivity and specificity depended on the cutoff value. A cutoff of >2100 pg/mL yielded sensitivity of 62.5% (95% CI, 43.69%-78.9%) and specificity of 85.71% (95% CI, 71.46%-94.57%), and a cutoff of >9000 pg/mL yielded sensitivity of 46.9% (95% CI, 29.09%-65.26%) and specificity of 97.62% (95% CI, 87.43%-99.94%). The authors concluded that synovial IL-6 is a more accurate marker than synovial WBC count.Table 2 and Figure 3 provide a concise review of the findings of each study.
Leukocyte Esterase
LE strips are an inexpensive screening tool for PJI, according to some studies. In a prospective clinical study of 364 endoprosthetic joint (hip, knee, shoulder) interventions, Guenther and colleagues13 collected synovial fluid before surgery. Samples were tested with graded LE strips using PJI criteria set by the authors. Results were correlated with preoperative synovial fluid aspirations, serum CRP level, serum WBC count, and intraoperative histopathologic and microbiological findings. Whereas 293 (93.31%) of the 314 aseptic cases had negative test strip readings, 100% of the 50 infected cases were positive. LE had sensitivity of 100%, specificity of 96.5%, PPV of 82%, and NPV of 100%.
Wetters et al14 performed a prospective clinical study on 223 patients who underwent TKAs and THAs for suspected PJI based on having criteria defined by the authors of the study. Synovial fluid samples were collected either preoperatively or intraoperatively.
Using a synovial fluid WBC >3k WBC per microliter, the sensitivity, specificity, PPV, and NPV were 92.9%, 88.8%, 75%, and 97.2%, respectively. Using positive cultures or the presence of a draining sinus tract, the sensitivity, specificity, PPV, and NPV were 93.3%, 77%, 37.8%, and 98.7%, respectively. Of note, the most common organism found at the time of revision for infection was coagulase-negative Staphylococcus (6 out of 39).Other authors have reported different findings that LE is an unreliable marker in PJI diagnosis. In one prospective clinical study of 85 patients who underwent primary or revision TSA, synovial fluid was collected during surgery.15 According to MSIS criteria, only 5 positive LE results predicted PJI among 21 primary and revision patients with positive cultures. Of the 7 revision patients who met the MSIS criteria for PJI, only 2 had a positive LE test. LE had sensitivity of 28.6%, specificity of 63.6%, PPV of 28.6%, and NPV of 87.5%. Six of the 7 revision patients grew P acnes. These results showed that LE was unreliable in detecting shoulder PJI.15
In another prospective clinical study, Tischler and colleagues16 enrolled 189 patients who underwent revision TKA or THA for aseptic failure or PJI as defined by the MSIS criteria. Synovial fluid was collected intraoperatively.
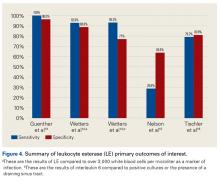
Fifteen of the 52 patients with a MSIS defined PJI had positive cultures with the most common organism being coagulase-negative Staphylococcus (7). Two thresholds were used to consider a positive LE test. When using the first threshold that had a lower acceptance level for positivity, the sensitivity, specificity, PPV, and NPV were 79.2% (95% CI, 65.9%-89.2%), 80.8 (95% CI, 73.3%-87.1%), 61.8% (95% CI, 49.2%-73.3%), and 90.1% (95% CI, 84.3%-95.4%), respectively. When using the higher threshold, the sensitivity, specificity, PPV, and NPV were 66% (95% CI, 51.7%-78.5%), 97.1% (95% CI, 92.6%-99.2%), 89.7% (95% CI, 75.8%-97.1%), and 88% (95% CI, 81.7%-92.7%), respectively. Once again, these results were in line with LE not being a reliable marker in diagnosing PJI.Table 3 and Figure 4 provide a concise review of the findings of each study.