Implementation of a resident handoff program at nine hospitals reduced both medical errors and preventable adverse events, according to a study published Nov. 5 in the New England Journal of Medicine.
Dr. Amy J. Starmer of Boston Children’s Hospital and her coinvestigators at dozens of other institutions implemented an I-PASS-based program in nine pediatric residency training programs in the United States and Canada from 2011 through 2013. I-PASS, a mnemonic to standardize handoffs, stands for illness severity; patient summary; action list; situation awareness and contingency plans; and synthesis by receiver. Study sites ranged in size from 36 to 182 residents (N. Engl. J. Med. 2014;371:1803-12).
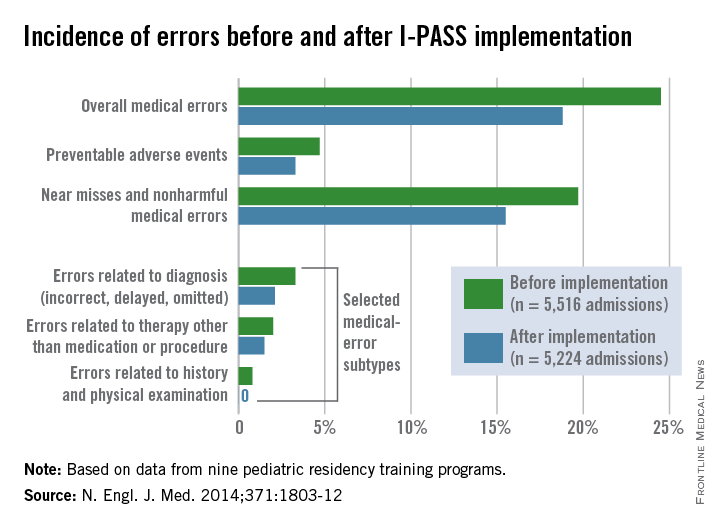
Of 10,740 patient admissions, the rate of medical errors decreased from 24.5 per 100 admissions preintervention to 18.8 per 100 admissions postintervention (23%), Dr. Starmer and her colleagues wrote. The rate of preventable adverse events fell from 4.7 events per 100 admissions to 3.3 events per 100 admissions (30%). Additionally, the rate of near misses and nonharmful medical errors went down by 21%. Investigators found no significant change in the rate of nonpreventable adverse events.
The I-PASS Handoff Bundle consisted of the I-PASS mnemonic; a 2-hour workshop on teamwork, communication skills, and I-PASS handoff techniques; a 1-hour role-playing session; a computer module; a faculty development program; direct-observation tools; and a process and culture-change campaign. Each site was assigned to one of three staggered intervention and data-collection waves from January 2011 through May 2013.
The hospitals integrated the I-PASS structure into both oral and written handoff processes. At seven sites, written handoff tools with a standardized I-PASS format were built into electronic medical record programs. The tools were built into word processing programs at two sites. Each hospital maintained an implementation log that was regularly reviewed to ensure adherence to program components.
Researchers found no significant time change in residents’ workflow after program implementation, including the time in a 24-hour period spent with patients and families.
Following the intervention period, the proportion of residents who rated the overall quality of their handoff training as very good or excellent rose from 28% to 72%.
“Implementing handoff improvement programs such as the I-PASS Handoff Bundle may potentiate the effectiveness of work-hour reductions, because doing both together may concurrently reduce both fatigue and handoff-related errors,” the study authors said.
The study was funded by the Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services, and others. The investigators reported no relevant conflicts of interest. Boston Children’s Hospital and the main study investigators are exploring the potential licensing of I-PASS.
On Twitter @legal_med