A basic understanding of the clinical components of musculoskeletal medicine is necessary in many medical fields. Musculoskeletal injuries represent the second most common presentation in US emergency departments, account for 49 million visits to orthopedic surgeon offices, and cost the United States an estimated $950 billion annually.1-3 Despite the staggering need for competency in musculoskeletal medicine, Freedman and Bernstein4 in 1998 demonstrated that musculoskeletal knowledge is inadequate among medical school graduates.
In 2005, the United States Bone and Joint Decade (now the United States Bone and Joint Initiative) announced Project 100, which recommended that 100% of US medical schools begin requiring a musculoskeletal course by the end of the decade.5 This project was intended to increase musculoskeletal understanding among medical students. Optimal curriculum reform, however, remains controversial. Many studies have found that medical schools continue to provide inadequate musculoskeletal education.4,6-9 For example, an integrated musculoskeletal curriculum with increased lecture time was found to improve clinical confidence but not musculoskeletal knowledge.6 In contrast, a 2-week intensive musculoskeletal module and a 6-week course involving orthopedic resident and faculty education has been shown to improve understanding.10,11
We conducted a study to determine the adequacy of musculoskeletal knowledge in medical school students, to determine musculoskeletal competency after curriculum reform through increased lecture and laboratory time, and to draw conclusions about factors leading to increased musculoskeletal competency to guide future curriculum reforms. We hypothesized that musculoskeletal knowledge would increase as a result of increased lecture and laboratory time.
Materials and Methods
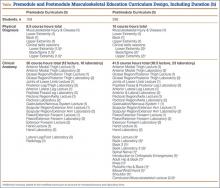
The Tufts University School of Medicine Institutional Review Board approved this study. The medical school curriculum at our institution was redesigned to include a dedicated musculoskeletal module to improve medical student education (Table). The study compared medical students given the old musculoskeletal module (premodule group) and those given the new musculoskeletal module (postmodule group). The premodule group received 8.5 hours of physical diagnosis skills training and 30 hours of clinical anatomy training (12 lecture hours, 18 laboratory hours), and the postmodule group received 10 hours of physical diagnosis training and 41.5 hours of clinical anatomy training (18.5 lecture hours, 23 laboratory hours).
The lecture material for the postmodule group covered all topics/questions addressed on the validated musculoskeletal adequacy assessment. The new module specifically added 6 hours of dedicated clinically based musculoskeletal lecture time during the anatomy course and concurrent with the physical diagnosis course. The topics covered with case-based scenarios were orthopedic emergencies, adult hip and back, knee, pediatric hip and back, elbow/wrist/hand, and shoulder. A validated musculoskeletal competency examination was given to the premodule group at the end of the musculoskeletal anatomy and physical diagnosis lectures. The postmodule group took the competency examination at the end of the “new” 6 hours of musculoskeletal education.
We used the Freedman and Bernstein4 basic competency examination for musculoskeletal education assessment to assess knowledge. This examination is the only validated tool for assessing basic clinical musculoskeletal knowledge. All students were also asked whether they had experience rotating in orthopedic surgery or in a related musculoskeletal field (rheumatology, physiatry, neurology) during the medical school “selective” period that allowed 1 afternoon per week of elective time. Duration of exposure was assessed. The examination was given to 109 students in the premodule group 1 year before the curriculum changes. The examination was then given to the students for the first 2 years after the curriculum changes were implemented, with 296 students in the postmodule group. All questions on the examination were addressed within the 6 lecture hours in the new module. A single reviewer anonymously scored the examinations according to the validated scoring system over a 2-week period.4 Independent t tests were used to compare examination scores between the premodule and postmodule groups. Statistical significance was set at P < .05. Equal variance between groups was not assumed.
Results
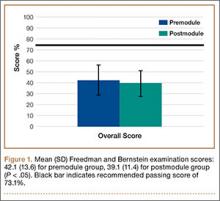
The examination was given to 405 medical students (109 premodule, 296 postmodule) Mean examination score was 40%, significantly below the recommended mean passing score of 73.1%.4 Only 1 student achieved a passing score. Independent t tests were used to compare examination scores of the premodule and postmodule groups. Mean (SD) scores were higher (P < .05) for the premodule group, 42.1 (13.6), than the postmodule group, 39.1 (11.4) (Figure 1).
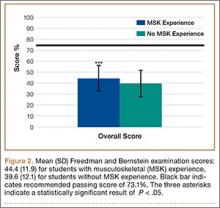
Independent t tests were used to compare examination scores of students with either orthopedics or rheumatology experience and students without this experience. Mean (SD) scores were higher (P < .05) for students with experience, 44.4 (11.9), than students without experience, 39.6 (12.1) (Figure 2). Students with neurology or physiatry experience did not score significantly higher than students without this experience. Statistical significance was set as P < .05. SAS 9.0 software (SAS Institute, Cary, North Carolina) was used for statistical analysis.