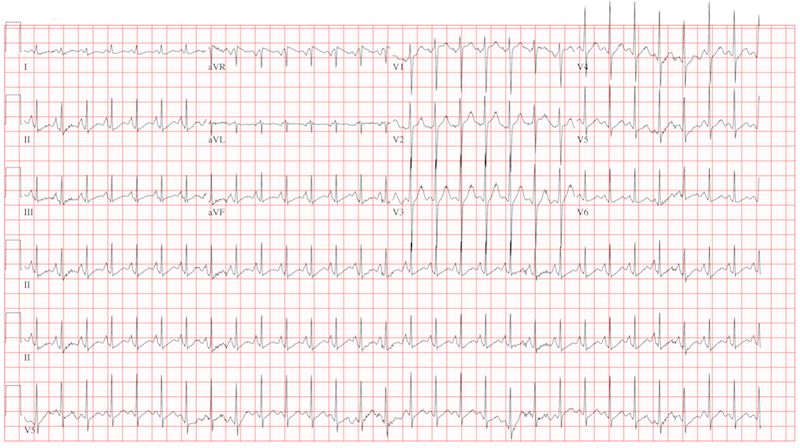
ANSWER
The correct interpretation is sinus tachycardia with a short PR interval. This ECG illustrates a physiologic sinus rate response to hypercarbic respiratory failure secondary to an infectious exacerbation. A shortened PR interval occurs with an otherwise healthy conduction system in response to a rapid sinus tachycardia.
Worsening Symptoms in Woman with Cystic Fibrosis
Lyle W. Larson, PhD, PA-C
A 23-year-old woman with cystic fibrosis presents to the pulmonary medicine clinic for follow-up to a hospitalization one month ago for an infectious exacerbation of her condition. She has had four hospital admissions over the past year and is known to be chronically colonized with multidrug resistant Pseudomonas. Two days ago, she began feeling significantly more short of breath, with increasing home oxygen requirements (4 L at baseline, up to 10 L by nasal cannula), as well as increasing phlegm production and a fever of 100°F. She states she feels dehydrated, sleepy, and nauseous. In addition to cystic fibrosis, her medical history is remarkable for pancreatic insufficiency, diabetes, chronic sinus infections, and bronchiolitis obliterans syndrome. Family history is positive for hyperlipidemia and congestive heart failure. No other family members have a diagnosis of cystic fibrosis. Her medication list includes azithromycin, insulin glargine, insulin isophane, insulin lispro sliding scale, insulin regular, loratadine, omeprazole, pancrelipase, prednisone, simvastatin, sulfamethoxazole-trimethoprim, and a tobramycin inhaler. She is allergic to cephalosporin antibiotics. A quick review of systems reveals no other issues. Physical examination reveals a woman in extreme distress who is able to nod to questions and answer briefly but is unable to speak in full sentences. Her blood pressure is 136/82 mm Hg, with a mean arterial pressure of 99 mm Hg; pulse, 170 beats/min and thready; respiratory rate, 40 breaths/min-1; and temperature, 39.2°C. O2 saturation is 89% on 10 L of oxygen via facemask. The pulmonary exam reveals coarse bilateral crackles, worst at the bases, with associated intercostal and supraclavicular muscular retractions. The cardiac exam reveals no jugular venous distention. Her rate is rapid and regular with no murmurs, rubs, or gallops. The abdomen is soft and nontender, with normal bowel sounds. The extremities are warm, well perfused, and without edema. The neurologic exam is grossly normal without focal signs. A stat arterial blood gas reveals respiratory acidosis with a pH of 7.32 and a pCO2 of 83 mm Hg. A complete blood count reveals a white blood cell count of 34 x 109/L. You decide to admit her to the medical intensive care unit. You are concerned that her heart rate of 170 beats/min may be atrial flutter and obtain an ECG, which reveals the following: a ventricular rate of 177 beats/min; PR interval, 88 ms; QRS duration, 60 ms; QT/QTc interval, 238/408 ms; P axis, 67°; R axis, 76°; and T axis, 73°. What is your diagnosis?