An estimated 1% to 2% of patients with chronic hypertension will at some time develop hypertensive urgency or emergency.1 According to recent data from the National Health and Nutrition Examination Survey (NHANES) 1999 to 2010,2 the prevalence of hypertension has remained stable at 30.5% among men and 28.5% among women in the United States; however, 74% of the hypertensive population is unaware of having this condition. Furthermore, 71.6% of hypertensive patients are managed for the condition, and in only 46.5% is blood pressure well controlled.2
In 2006, essential hypertension was estimated to account for more than 44 million emergency department visits in the US. The direct and indirect costs of hypertension totaled $73 billion in 2009.3,4
NEW TERMINOLOGY AND CLASSIFICATION
The terms malignant hypertension, hypertensive crisis, and accelerated hypertension have been replaced by hypertensive urgency or hypertensive emergency. Hypertensive urgency and emergency are differentiated by the absence or presence of acute end-organ damage, respectively.
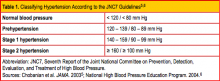
Given the inconsistent terminology used, database searches can be challenging. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7),5,6 published in 2003, is considered the gold standard for categorizing hypertension in the outpatient setting. The JNC7 authorsclassify normal blood pressure as < 120/< 80 mm Hg. The document further classifies blood pressure into the stages shown in Table 1.5,6 Blood pressure higher than 180 mm Hg systolic and/or 120 mm Hg diastolic is generally considered severe hypertension— a designation that includes hypertensive urgency and hypertensive emergency.6
What Defines Hypertensive Urgency/Emergency?
Hypertensive urgency is defined as a diastolic blood pressure of 110 mm Hg or greater without the acute signs of end-organ damage.7 Some sources suggest that a patient must also have certain risk factors (eg, heart disease, renal disease) to be given this diagnosis.8 The presence of acute and rapidly evolving end-organ damage with an elevated diastolic blood pressure, usually greater than 120 mm Hg, establishes a diagnosis of hypertensive emergency.6,8,9
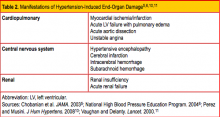
No specific blood pressure measurement indicates a hypertensive emergency, however; rather, the defining feature of this diagnosis is the presence of progressive target end-organ damage.7 This is most commonly manifested in cardiopulmonary, central nervous system, and/or renal findings; for the specific forms of end-organ damage, see Table 2.5,6,10,11 Preeclampsia and eclampsia are also considered manifestations of hypertensive end-organ damage but are beyond the scope of this article.5,11
The most common form of organ damage associated with hypertension is ischemic heart disease, in the form of either heart failure or acute coronary syndrome.12
PATHOPHYSIOLOGY
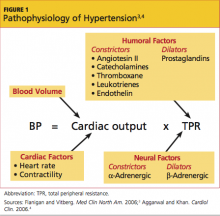
Blood pressure is calculated by cardiac output (ie, stroke volume multiplied by heart rate) multiplied by total peripheral resistance. Total peripheral resistance is influenced by a variety of humoral and neural factors, also known as vasoactive substances (see Figure 13,4). During an episode of acute hypertension, a failure of autoregulatory function occurs, precipitated by one or more of a host of potential causes. This failure of autoregulation then leads to increased systemic vascular resistance. In the setting of end-organ damage, release of inflammatory markers ensues, which ultimately causes endovascular injury and fibrin necrosis of arterioles.4,10,11
The renin-angiotensin-aldosterone system also plays a significant role in the cascade of hypertension, stimulating decreased renal perfusion and lowering tubular sodium concentration. This in turn stimulates aldosterone to increase blood pressure by maintaining excess volume through sodium retention and potassium excretion, further potentiating the cycle of uncontrolled blood pressure.4,13,14
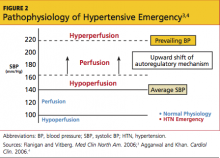
Patients with chronically elevated blood pressures have a compensatory response, lying in the threshold mechanism, that protects against end-organ damage. Acute changes in blood pressure are better tolerated in these patients because of their decreased propensity for hypoperfusion.4 In contrast, normotensive patients who experience precipitous changes in blood pressure are at increased risk for organ hypoperfusion. The main concern regarding organ hypoperfusion is that it can lead to ischemia4 (see Figure 23,4).
PATIENT HISTORY
Acute hypertensive urgency or emergency can be triggered by many factors. Systemic etiologies (including kidney disease) caused by immunologic mediators or renal artery stenosis can cause or exacerbate hypertension. The patient should be asked about his or her normal blood pressure range, as this may offer clues to medication compliance. Rebound hypertension can be seen in patients who abruptly discontinue medications such as clonidine or β-blockers, as this causes an increase in sympathetic outflow.9,15
All patients should be queried regarding their use of OTC medications and other drug use, including cocaine, methamphetamines, phencyclidine, and alcohol.1,4,11,16 Patients taking monoamine oxidase inhibitors (MAOIs) are at increased risk for serious medication interactions; concomitant administration of MAOIs with other antidepressants can lead to a hypertensive reaction, but also to serotonin syndrome.1,17 Because MAOIs inhibit the breakdown of tyramine, patients taking them should avoid tyramine-containing foods and herbal supplements (including, but not limited to, St. John's wort, ginseng, and yohimbine).1,15,18