Goal-directed therapy is initiated even before the patient evaluation has been fully completed. Patient assessment continues after treatment is begun to avoid overly aggressive blood pressure reduction, which can increase the risk for patient demise or morbidity.4
Exceptions in the treatment of hypertensive emergencies (particularly of specific disease states) will be discussed below, along with other treatment considerations. Patient comorbidities, for example, must be considered in the choice of antihypertensive agents.
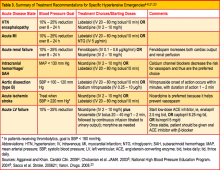
Focused Treatment for Specific Hypertensive Emergencies
Hypertensive encephalopathy. This condition, associated with severe hypertension, is indicated by an abrupt change in mental status. During this acute end-organ damage event, a failure of cerebral autoregulation occurs, with increased pressure in the vascular endothelium leading to arteriole dilation that in turn can result in hyperperfusion of the brain, cerebral edema, and microhemorrhages.23
Because presentation of hypertensive encephalopathy may be similar to that in patients with acute stroke, hemorrhage, or brain lesions, these and other potential causes must be ruled out. While blood pressure treatment goals correspond with general recommendations,5,6 caution must be taken not to reduce blood pressure too swiftly; thus, continuous monitoring is warranted. If the patient's neurologic function worsens, treatment should be suspended and blood pressure allowed to rise slowly.4
Preferred antihypertensives for patients with hypertensive encephalopathy include labetalol, nicardipine, and fenoldopam23 (see Table 34-6,21,23). Centrally acting antihypertensives, such as clonidine, methyldopa, or reserpine,24 should not be used, as they can cause central nervous system depression and may cloud the patient's sensorium further.
Myocardial ischemia/infarction. During an acute hypertensive event, the workload on the heart and activation of the renin-angiotensin-aldosterone system can lead to acute coronary ischemia or infarction.23 Treatment is aimed at increasing blood flow to the myocardium and reducing the workload on the heart. Antihypertensives are combined with reperfusion (eg, angioplasty) and/or thrombolytics to preserve myocardial structure and function. Standard agents to reduce blood pressure include IV nitroglycerin and β-blockers. Systolic blood pressure is reduced until symptoms subside or diastolic blood pressure is reduced to 100 mm Hg or lower. Adjuncts such as morphine and oxygen are used to reduce patient discomfort and improve oxygen delivery to the myocardium.4
Acute left ventricular failure. In this potential manifestation of hypertensive emergency, the left ventricle initially attempts to compensate for rising blood pressure and becomes hypertrophic. Once the myocardium can no longer meet the demand, left ventricular function decompensates, causing a flow backup that leads to acute pulmonary edema.23
Blood pressure goals mirror those in the general treatment recommendations but focus specifically on reducing preload and afterload, improving myocardial contractility and decreasing peripheral vascular resistance. The preferred agents in this setting are IV nitroglycerin and ACE inhibitors, along with loop diuretics, morphine, and oxygen.4 Medications that increase workload on the heart (eg, hydralazine, clonidine) should be avoided.23
Aortic dissection. This is a true medical emergency that can result in significant morbidity and mortality. Type A dissection occurs proximally, at the ascending aorta, whereas type B dissection occurs at the level of the descending aorta. Typically, type B dissection is managed medically, as surgical treatment carries a significant risk for paralysis.4 Both types of aortic dissection are strongly associated with uncontrolled hypertension and in some patients may be precipitated by an acute hypertensive event. In such cases, the goal for blood pressure reduction is to decrease the shearing forces associated with the dissection. This is accomplished by lowering both blood pressure and pulse rate.12
While cases of type A dissection are usually managed surgically, all affected patients will require some component of medical management and tight blood pressure control. The current recommendation for blood pressure in aortic dissection is swift downward titration to a goal systolic blood pressure of 100 to 110 mm Hg.4 A β-blocker in combination with a vasodilator, administered intravenously, should be used for swift blood pressure reduction.4,25
IV nitroprusside, a potent vasodilator, is the preferred agent, but its use requires intra-arterial blood pressure monitoring.23 Because nitroprusside is metabolized to cyanide, its use can lead to lethal toxicity, especially in patients with hepatic or renal impairment.11 In this patient population, IV labetalol or esmolol may be used instead.4,25
Acute renal failure. In the setting of an acute hypertensive episode, it is often difficult to determine whether acute renal failure is the cause or the effect. Regardless, rapid reduction in blood pressure is warranted to preserve renal function and to stop the cycle of microvascular kidney destruction. Blood pressure goals are aligned with the general treatment recommendations. The preferred antihypertensive agent is IV fenoldopam, a dopamine receptor agonist that directly dilates renal arterioles, improving renal perfusion and promoting diuresis.4,26 Nicardipine, a calcium channel blocker, may be considered as an alternative.23,27