According to the US Centers for Disease Control and Prevention (CDC), in 2011 there were 25.8 million people in the United States living with diabetes mellitus (DM), 90% to 95% of whom had type 2 DM.1 Seven million of those with DM are undiagnosed. In addition, an estimated 79 million adults in the United States have prediabetes, a condition in which glycated hemoglobin (HbA1c) levels are above normal but do not yet meet the diagnostic threshold for DM (≥6.5%).1 This large population with prediabetes, defined by HbA1c levels of 5.7% to 6.4%, has a 5-year risk of progression to diabetes ranging from 9% to 50%; the higher risk is associated with higher HbA1c levels as the disease represents a continuum.2
The benefits of diagnosis and treatment of diabetes—preventing the progression of microvascular complications—are well established. Through medication, exercise, and dietary interventions, the progression of both prediabetes and diabetes can be halted and in many cases reversed.
Given the prevalence of DM in the United States and the clear benefits of treatment, the ability to diagnose DM is important for any physician who may encounter patients with undiagnosed diabetes or prediabetes. This article reviews the management of hyperglycemia relevant to the emergency physician (EP) and discusses the criteria used in diagnosing DM.
The American College of Emergency Physicians (ACEP) currently does not have a clinical policy for the initial treatment of patients with DM that is newly diagnosed in the ED. A 2007 survey of 152 EPs in the United States found that 52% would leave initiation of outpatient treatment of diabetes to a patient’s primary care physician (PCP), regardless of the degree of hyperglycemia noted in the ED.3 Almost paradoxically, among these same EPs, the most common reason for not screening for diabetes (cited by 69%) was the inability to secure follow-up for newly diagnosed patients. Given the fragmentary care many emergency patients receive and the difficulty in assuring close ED follow-up, reviewing the American Diabetes Association (ADA) recommendations for initiation of diabetes management is worthwhile.
ADA Treatment Guidelines
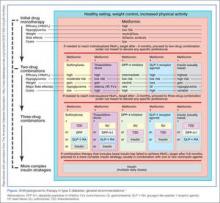
The ADA-recommended strategy for the outpatient treatment of DM is illustrated in the Figure.4 Lifestyle interventions, including a healthy diet, weight loss, and increased physical activity, are at least as effective as any individual pharmacotherapy in decreasing HbA1c.Metformin
Metformin, if tolerated and without contraindications, is the preferred initial pharmacologic agent for all patients with newly diagnosed DM. This drug typically lowers HbA1c by 1.5%, and does not cause weight gain or hypoglycemia associated with some other oral agents (eg, sulfonylureas). Metformin therapy, however, is contraindicated in patients with chronic kidney disease (CKD) (Cr >1.5 in males and >1.4 in females), liver disease, a history of lactic acidosis, and a low-perfusion state. Metformin also should not be used for 48 hours following an intravenous (IV) contrast-enhanced study.
When starting metformin or increasing the dose, patients frequently experience abdominal symptoms, including cramping, nausea, vomiting, and diarrhea. These side effects are usually mild and self-limiting, and they usually resolve within a week. However, patients should be warned of these complications and advised to take metformin with meals to limit side effects. They also should be encouraged to continue the medication through the initial symptoms, if possible.
For a patient with newly diagnosed type 2 DM, a reasonable ED discharge plan is to start metformin at 500 mg daily, taken with a meal. If the patient develops abdominal symptoms, the dose can be reduced to 250 mg daily. Patients should additionally be advised to follow up with their PCP as soon as feasible. Patients can be instructed to increase the dose of metformin on their own. Because the development of gastrointestinal symptoms is the main dose-limiting effect of metformin therapy, it is generally safe to give patients instructions on weekly dose escalation by 500 mg/day to the optimal dose of 1,000 mg twice daily. Although metformin therapy is associated with rare cases of lactic acidosis in patients with CKD, it does not, on its own, cause acute kidney injury; therefore, intense monitoring is not required while doses are increased. Metformin therapy can decrease vitamin B12 absorption, though it rarely results in megaloblastic anemia, and it takes 5 to 10 years for neurological symptoms to manifest.5
Other Treatment Options
The Figure highlights the ADA guidelines on additional pharmacologic agents beyond metformin. When these additional agents are used, the patient should follow-up with a PCP every 3 months to determine how far HbA1c has been lowered. For most patients with DM, the goal for HbA1c is less than 7%. This goal may be raised for elderly patients and those with a history of cardiovascular disease, as these patients are at higher risk for cardiovascular mortality from an episode of hypoglycemia.