The preferred insulin regimen for noncritically ill diabetic inpatients consists of scheduled subcutaneous therapy with basal, nutritional, and correctional components.9 Because absorption from subcutaneous tissue varies among critically ill patients, the ADA recommends an IV insulin therapy protocol for ICU patients with diabetes. The NICE SUGAR trial found that the overall risk of death was 2.6% higher among patients treated with an intensive insulin therapy regimen (finger stick blood glucose goal 80-108 mg/dL) than it was among patients treated using standard therapy with a goal of less than 180 mg/dL, a statistically significant difference.10 These results form the basis for the ADA-recommended inpatient glycemic target of 140 to 180 mg/dL among critically ill patients.11 While no definitive evidence exists to guide glycemic control among noncritically ill inpatients, the strategy applied to critically ill patients can be extrapolated to other hospitalized patients because the ADA recommends treatment to keep finger stick blood glucose values below 180 mg/dL.
Hypoglycemia
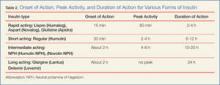
No discussion of hyperglycemia or DM is complete without a discussion of hypoglycemia. Because symptoms due to hypoglycemia frequently trigger ED evaluation, it is worthwhile for the practicing EP to periodically review the timing profile of the insulin preparations currently in use (Table 2). According to the ADA, for patients with diabetes, hypoglycemic unawareness or any significant hypoglycemic event should automatically trigger a medication re-evaluation.Often a hypoglycemic event can clearly be correlated to a missed meal. This may only require re-education of the patient about the need to be consistent in the timing of his or her dietary regimen. However, often a hypoglycemic event is not clearly related to a missed meal. When a patient has recently taken a long-acting insulin or sulfonylurea or has new renal failure, prolonged observation or admission may be required. In most other cases of medication-induced hypoglycemia, the patients are expediently sent home. As many such patient encounters occur in the early morning hours, EPs need to know how to manage insulin regimens if these patients are to be safely discharged home. Additionally, worsening renal function is a common cause of potentiation of both oral agents and insulin; it is generally worthwhile to check renal function on patients presenting with significant hypoglycemia.
After a significant hypoglycemic event, many guidelines recommend decreasing the daily insulin dose by 10% to 20%. However, with a careful medication history and knowledge of each insulin dose’s activity profile, a physician can often discern which individual insulin dose is responsible for a given hypoglycemic event. That individual daily dose can then be decreased by 20% to better target the cause of the hypoglycemic event.
Conclusion
Diabetes mellitus is one of the most common chronic medical conditions in the United States, and more than 7 million Americans may be living with undiagnosed DM. In the ED setting, physicians regularly encounter patients with undiagnosed type 2 DM. Since treatment is known to prevent the microvascular complications associated with DM, EPs should know the diagnostic criteria and understand the ADA’s inpatient and outpatient treatment recommendations.