News

AT AN NIH CONSENSUS DEVELOPMENT CONFERENCE
BETHESDA, MD. – The current two-step method of diagnosing gestational diabetes mellitus in U.S. pregnant women will not change, based on the recommendations of an independent, voluntary panel at a National Institutes of Health Consensus Development Conference.
The panel released their statement March 6, following the 3-day NIH Consensus Development Conference on Diagnosing Gestational Diabetes Mellitus, during which expert and public comments were incorporated into the draft consensus statement.
The conference convened to review the evidence on gestational diabetes mellitus (GDM) diagnosis methods and discuss seven questions regarding the possible adoption of a recommendation for the single-step approach to diagnosing the condition rather than the two-step method currently used most commonly in the United States.
The one-step approach was proposed by the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) following a 2008 study suggesting that thousands of women are adversely affected by subclinical hyperglycemia. The independent NIH panel, however, determined that additional research is necessary before recommending the single-step method.
"At present, the panel believes that there is not sufficient evidence to adopt a one-step approach, such as that proposed by the IADPSG," the panel wrote. "The panel is particularly concerned about the adoption of new criteria that would increase the prevalence of GDM, and the corresponding costs and interventions, without clear demonstration of improvements in the most clinically important health and patient-centered outcomes."
GDM currently affects approximately 5%-6% of all U.S. pregnancies, including more than 240,000 pregnant women, according to the NIH. This prevalence, however, is based on the use of the current two-step test, and widespread implementation of the single-step test under consideration would likely increase the number of women diagnosed with GDM by two to three times.
A variety of methods exist for screening women for GDM, depending on whether fasting is required, how many grams of glucose the woman consumes for the test, how many appointments the screening requires, and what glucose threshold is used for diagnosis.
The most commonly used method in the United States, recommended by the American College of Obstetricians and Gynecologists, is a two-step method conducted when women are 24-28 weeks pregnant. Women’s blood glucose levels are initially tested 1 hour after consumption of a 50-g glucose drink. If the test indicates a blood glucose level of 130 mg/dL or greater on that test, she undergoes a 3-hour 100-g glucose tolerance test. GDM is diagnosed if a woman’s blood glucose levels reach at least two of the following thresholds: 95 mg/dL after fasting, 180 mg/dL at 1 hour, 155 mg/dL at 2 hours, or 140 mg/dL at 3 hours.
The single-step method involves a fasting plasma glucose and a 75-g 2-hour test between 24 and 28 weeks of pregnancy. A result of at least 92 mg/dL at fasting, 180 mg/dL at 1 hour, or 153 mg/dL at 2 hours would be the threshold for diagnosis of GDM.
The single-step approach is supported by the American Diabetes Association and the World Health Organization (with 110 mg/dL at fasting and 140 mg/dL at 2 hours) and is used in a number of other countries.
However, several doctors have raised concerns that moving to the single-step approach could lead to more interventions for a much larger number of pregnant women who would now be diagnosed, increasing possible harms and costs.
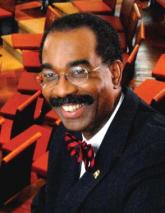
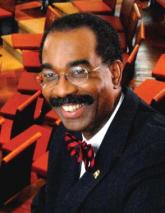
Dr. Peter VanDorsten, the conference panel chairperson and Lawrence L. Hester, Jr. Professor at the Medical University of South Carolina, Charleston, said the research indicates that using the single-step method would increase the number of women diagnosed with GDM to 15%-20% of all pregnancies.
On the plus side, more diagnoses would result in more treatment for these women, which could include nutritional and lifestyle counseling, more clinic visits, and possible insulin therapy. Possible complications associated with GDM include preeclampsia, cesarean delivery, macrosomia, shoulder dystocia, and birth injuries to the mother. Women diagnosed with GDM are also 35%-60% more likely to develop type 2 diabetes later. Babies born to women with GDM are also at a higher risk for hypoglycemia, jaundice, and having difficulty breathing at birth.
On the other hand, more diagnoses would result in higher health care costs and more interventions for women, which could lead to possible harms.
"There is also evidence in some studies that the labeling of these women may have unintended consequences, such as an increase in cesarean delivery and more intensive newborn assessments," the panel wrote in their statement. "In addition, increased patient costs, life disruptions, and psychosocial burdens have been identified. Currently available studies do not provide clear evidence that a one-step approach is cost-effective in comparison with the current two-step approach."