Eradicating Helicobacter pylori bacteria with a short course of antibiotics and proton pump inhibitors helped reduce the risk of gastric cancer in otherwise healthy and asymptomatic H. pylori–positive adults by 34%, according to a review published online July 22.
However, because all but one of the six studies included in the analysis were conducted in Asian populations, it is not known whether the results would be the same in Western populations.
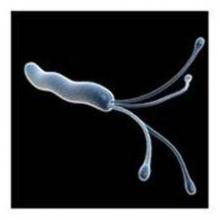
“Gastric cancer is the third most common cause of cancer death worldwide,” wrote the researchers, who are members of the Cochrane Upper Gastrointestinal and Pancreatic Diseases Group. “Individuals infected with H. pylori have a higher likelihood of developing gastric cancer than individuals who are not infected. Eradication of H. pylori in healthy asymptomatic individuals in the general population may reduce the incidence of gastric cancer, but the magnitude of this effect is unclear.”
For the review, the researchers searched the Cochrane Central Register of Controlled Trials and other major databases for randomized, controlled trials that compared at least 1 week of H. pylori therapy with placebo or no treatment in preventing subsequent development of gastric cancer in otherwise healthy and asymptomatic H. pylori–positive adults (Cochrane Database Syst. Rev. 2015 [doi:10.1002/14651858.CD005583.pub2]. To be included, trials had to follow up participants for at least 2 years and needed to have at least two participants with gastric cancer as an outcome. The researchers defined gastric cancer as any gastric adenocarcinoma, including intestinal (differentiated) or diffuse (undifferentiated) type, with or without specified histology.
In all, six studies with a total of 6,497 participants met eligibility criteria. The studies primarily used a combination of antibiotics and proton pump inhibitors. Five of the six studies were conducted in Asian populations. Of 3,294 participants assigned to eradication therapy, 51 (1.6%) subsequently developed gastric cancer, compared with 76 (2.4%) of 3,203 participants who received placebo or no treatment. “There was no statistically significant heterogeneity between individual trial results,” the researchers wrote. “Therefore there was a small, but statistically significant benefit of H. pylori eradication therapy in preventing gastric cancer in healthy asymptomatic infected individuals (risk ratio, 0.66).”
They pointed out that the effect of H. pylori eradication on preventing death from gastric cancer, compared with placebo or no treatment “was uncertain due to wide confidence intervals” and there was “no evidence of an effect on all-cause mortality. Adverse events data were poorly reported.”
The researchers acknowledged certain limitations of the review, including that fact that only three of the trials were considered to be at low risk of bias. In addition, the design of some trials made it “difficult to ascertain whether the significant reduction in the risk of subsequent gastric cancer was due to H. pylori eradication therapy alone, or to the antioxidants or vitamins that were coadministered in some of the trials.”
In terms of implication for clinical practice, “the findings of this systematic review and meta-analysis add to the increasing evidence that eradicating H. pylori in the general population has the potential to prevent gastric cancer,” they concluded. “International guidelines for the management of H. pylori infection may change as a result.”
The researchers reported having no relevant financial conflicts.