SAN ANTONIO – Despite mounting evidence that blood cultures don’t contribute to the care of immunocompetent children admitted to the hospital with uncomplicated skin and soft tissue infections (SSTIs), they continue to be performed routinely in some hospitals, according to a study presented at the Pediatric Hospital Medicine 2015 meeting.
Current practice guidelines recommend against routine use of blood cultures in uncomplicated SSTIs (Clin Infect Dis. 2014;59(2):e10-52).
A 2013 study of children admitted for uncomplicated SSTIs (n = 482) found no positive blood cultures in the cohort, and cultures were also associated with a significantly longer length of stay. More than half of those children, however, had received antibiotics before their blood cultures, leaving open the possibility that some negative results were the result of treatment with antibiotics (Pediatrics. 2013;132(3):454-9).
Dr. Claudette Gonzalez and her colleagues at Nicklaus Children’s Hospital, Miami, presented findings from a study that used a cohort of otherwise healthy infants and children (n = 176) admitted from the emergency department with uncomplicated SSTIs.
Dr. Gonzalez and her associates sought to strengthen the evidence against routine use of cultures by excluding children who had received antibiotics within 2 weeks of presenting to the hospital.Dr. Gonzalez noted that, despite guidelines, blood cultures remained a routine part of the workup at her hospital, with 66% of the study sample receiving cultures (n = 116). Of febrile patients, 80% received cultures; of nonfebrile patients, 59% received cultures. Patients who had a blood culture drawn were significantly more likely to have had fever (P < .01). They also were more likely to have higher white blood cell and C-reactive protein (CRP) counts (P > .05 for both), but despite this, the rate of positive blood cultures was still less than 1%.
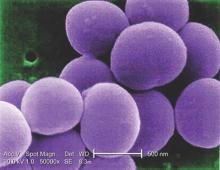
Of the 116 blood cultures drawn, 5 grew contaminants and only 1 was a true positive, for methicillin-susceptible Staphylococcus aureus (MSSA).
The study, unlike most previous studies, enrolled patients younger than 1 year of age (n = 28), but Dr. Gonzalez said that “we don’t have a big enough sample to really make conclusions about that age group.” Also in contrast to some previous studies, Dr. Gonzalez and her associates did not find a statistically significant difference in length of stay between the patients who had received cultures and those that did not (mean 3.62 vs. 3.4 days, P > .05).The one patient in the study with true bacteremia was a 1.4-year-old child presenting with no fever, cellulitis of hands and feet, no lymphangitis, and a white blood count of 8.5 × 103/L and a CRP of less than 0.5 mg/dL. “The WBC count was within normal range and the CRP was not elevated, so you wouldn’t have necessarily picked this kid out to say he needs a blood culture,” Dr. Gonzalez said at the meeting, which was sponsored by the Society of Hospital Medicine, the American Academy of Pediatrics, the AAP Section on Hospital Medicine, and the Academic Pediatric Association.
Still, she said, the study strengthens the evidence base against use of blood cultures in this population. “For children 1 year and older I think it’s very clear,” she said. The investigators are now proceeding with an implementation study to determine whether guidance against routine blood cultures should be put into practice at their institution.
Although the initial study revealed that 66% of children with uncomplicated SSTIs were receiving cultures, preliminary unpublished results show “it’s now at about 44%,” she said, following education of residents, fellows, and ED clinicians.
In addition to communicating with the ED to reduce use of blood cultures in this population, Dr. Gonzalez said, “we’re getting guidelines plugged into our order set in the [electronic medical record], so that’s a second reminder not to draw blood cultures. And we’re measuring to see if our rates improve further.”
Dr. Gonzalez received no outside funding for her study and disclosed no conflicts of interest.