A modified version of the cardiometabolic disease staging (CMDS) scoring system can be effectively used in a clinical setting to identify patients who are at an elevated risk for developing diabetes, according to a study published in the Journal of Clinical Endocrinology & Metabolism.
“To enhance the application of the CMDS system in clinical settings, we sought to develop a weighted scoring system based on risk factor components in the CMDS system for the prediction of future diabetes by separate identification and weighting of those risk components,” said Dr. Fangjian Guo of the University of Texas Medical Branch, Galveston, and Dr. W. Timothy Garvey of the University of Alabama, Birmingham.
The CMDS scoring method involves these measures:
• Fasting blood glucose of at least 100 mg/dL.
• Two-hour glucose from oral glucose tolerance test (OGTT) of at least 140 mg/dL.
• Waist circumference of 102 cm for men and 88 cm for women.
• Blood pressure (systolic of at least 130 mm Hg and/or diastolic of at least 85 mm Hg) or use of antihypertensive medication.
• HDL cholesterol under 40 mg/dL in men and under 50 mg/dL in women.
• Fasting triglycerides of at least 150 mg/dL or use of antihyperlipidemia medication.
Dr. Guo and Dr. Garvey used data from the CARDIA study and the ARIC study for their investigation.
CARDIA is a large, ongoing population study of 5,115 black and white adults, age 18-30 years, recruited from 1985 to 1986, with follow-up examinations conducted in seven visits over the next 25 years.
ARIC is an ongoing prospective cohort study of 15,792 men and women recruited at age 46-64 years in 1987 from either Mississippi, North Carolina, Minnesota, or Maryland, with follow-ups every 3 years.
The CMDS score was derived based on “verified incident diabetes cases from the CARDIA study” and was validated “in participants from the ARIC study,” after which the researchers “fitted Cox models and derived CMDS scores for diabetes accordingly,” the researchers wrote (J Clin Endocrinol Metab. 2015 Aug 4 doi: 10.1210/jc.2015-2691).
Overall, weighted diabetes CMDS scores were derived for 2,857 subjects and were validated in 6,425 subjects from the ARIC study. Scores in each of the six subcategories carried integer values that, when totaled, equaled a maximum of 100 per subject.
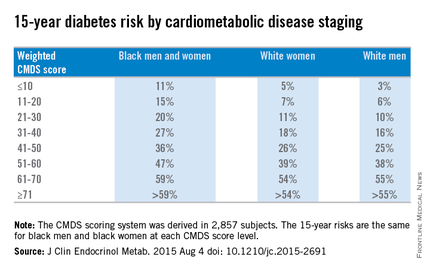
Weighted CMDS scores of 10 or lower were found to indicate a low 15-year risk of diabetes rate: 11% for both black men and women, 5% for white women, and 3% for white men. Weighted CMDS scores of 11-20 indicate a 15% risk for black men and women, 7% for white women, and 6% for white men. Scores of 21-30 indicated a 20% risk for black men and women, 11% for white women, and 10% for white men. Scores of 31-40 indicated a 27% risk for black men and women, 18% for white women, and 16% for white men. Scores of 41-50 indicated a 36% risk for black men and women, 26% for white women, and 25% for white men.
Fifteen-year diabetes-risk rates increased in the higher CMDS score brackets. In the 51-60 range, black men and women have a 47% risk, compared with 39% for white women and 38% for white men. Scores of 61-70 indicated a 59% risk for black men and women, 54% for white women, and 55% for white men. In the final score bracket of 71 and higher, the risk is greater than 59% for black men and women, greater than 54% for white women, and greater than 55% for white men.
“The main strength of this study is the development and validation of a weighted diabetes algorithm using data from two large prospective national cohorts,” Dr. Guo and Dr. Garvey noted, adding that “incident diabetes in the CARDIA study was based on rigorous measures of fasting glucose and 2-hour OGTT glucose, such that the ascertained diabetes cases provide a solid basis for the development of our weighted CMDS scoring system.”
Limitations of the study include the fact that blood glucose measures were not available for ARIC participants after the fourth visit and that diabetes cases were based on hospital records and self-reports. Furthermore, both CARDIA and ARIC looked exclusively at black and white subjects, meaning that other minority groups – particularly Asians – were not included.
This study was supported by the merit review program of the Department of Veterans Affairs, National Institutes of Health, and the UAB Diabetes Research Center. Dr. Guo is supported by an institutional training grant from the Eunice Kennedy Shriver National Institute of Child Health & Human Development at the NIH.