Over 30 million injuries were treated in U.S. emergency departments in 2013, costing an estimated $671 billion, the Centers for Disease Control and Prevention reported.
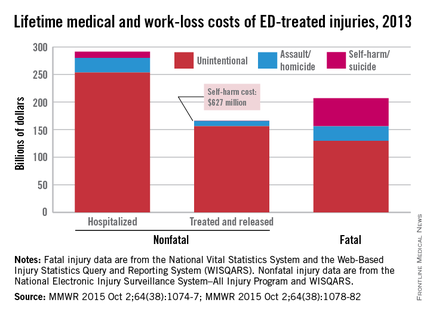
The largest share of that cost – almost $290 billion, or about 43% – came from the 3 million persons with nonfatal injuries who were hospitalized. Costs for the 27 million people who were treated and released from emergency departments were $167 billion, which was just under 25% of the total. The lifetime cost estimate for the almost 193,000 injury-associated deaths in 2013 was over $214 billion (32%), said Curtis Florence, Ph.D., of the CDC’s National Center for Injury Prevention and Control, Atlanta, and associates.
For each ED-treated injury-related death, the mean cost in terms of lost lifetime earnings and medical care provided was just over $1.1 million: Homicides cost over $1.6 million, suicides were $1.2 million each, and each unintentional injury death cost just under $1 million, they said (MMWR. 2015 Oct 2;64[38]:1074-77).
Drug poisonings, including prescription drug overdoses, accounted for the largest share of fatal injury costs (27%), followed by transportation-related deaths (23%) and firearm-related deaths (22%), Dr. Florence and associates noted.
The mean cost for each nonfatal injury (both hospitalized and treated and released from the ED) was $15,211. Self-harm injuries cost $25,121, compared with $23,034 for each assault and $14,685 for each unintentional injury (MMWR. 2015 Oct 2;64[38]:1078-82).
“Injuries cost Americans far too much money, suffering, and preventable death,” CDC Director Tom Frieden said in a written statement. “The doubling of deaths by drug poisoning, including prescription drug overdose and heroin, is particularly alarming.”
The investigators used data from the National Vital Statistics System and the Web-Based Injury Statistics Query and Reporting System (WISQARS) for injury-related deaths and the National Electronic Injury Surveillance System–All Injury Program and WISQARS for nonfatal injuries.