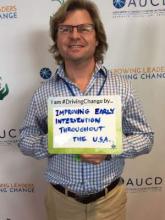
One of the perceived failings of the No Child Left Behind Act was that it attempted to address disparities by increasing standardized testing throughout the K-12 period. Ironically, it left children under 5 years … well, behind. To more effectively prevent problems and reduce disparities, our nation should improve its early detection and intervention system.
This means increasing standardized screening for developmental-behavioral problems or at-risk conditions from 0 through 5 years – and then, swiftly connecting at-risk children/families to the most effective and appropriate community services. This strategy is analogous to quickly detecting and putting out small fires before they morph into raging forest fires.
On Dec. 10, The Every Child Achieves Act of 2015 was signed into law by President Obama with bipartisan support. One seemingly minor, but important new change is that federal funds can be allocated for states, school districts, and schools to improve early childhood learning services. However, the extent to which different states invest in early childhood programs remains to be seen.
A month earlier, a Pediatrics article entitled “Systemwide Solutions to Improve Early Intervention for Developmental-Behavioral Concerns” offered expert advice on how to frugally invest those dollars (Pediatrics 2015 Nov. doi: 10.1542/peds.2015-1723). For children aged 0- 5 years, my coauthors and I proposed that every state needs:
• Systemwide screening and care coordination.
• Comprehensive, equitable, and tiered assessments for at-risk or referred children.
• Universal access to high-quality early learning or preschool programs.
• Continuous accountability for the early detection and intervention process.
Systemwide screening
The American Academy of Pediatrics (AAP), along with a federal-level initiative, Birth to 5: Watch Me Thrive! recommends every infant, toddler, and preschooler be periodically screened for developmental-behavioral problems. The new mantra is, “Learn the Signs. Act Early.”
Parents should know that high-quality screening does not prematurely label children with a diagnosis. Instead, regular screenings help raise awareness of their child’s development, making it easier to expect and celebrate developmental milestones. Very importantly, screening has also been proven to substantially improve the percentage of children receiving early intervention (EI).
Connecting the dots, high-quality EI substantially lowers rates of academic remediation or failure, teenage pregnancy, antisocial or criminal behavior, substance abuse, suicidal ideation and attempts, unemployment, and welfare dependency. Just think how preventing all these problems relates to what has been in the news recently.
In reality, many health care clinics, day care centers, and preschools still don’t offer high-quality screening. Even pediatricians can struggle with implementing the AAP’s recommendations . In a busy office, proper implementation requires teamwork. At a statewide level, entire populations need to be accurately screened and tracked.
Systemwide care coordination
Unfortunately, only about 50% of referred children are promptly connected to EI services (Clin Pediatr [Phila]. 2011 Sep;50[9]:853-68). Many overwhelmed or anxious parents don’t follow up. This is problematic because these same “lost to follow-up” children typically perform well below average and have numerous, predictive academic and psychosocial risk factors. Meanwhile, health care providers struggle with tracking at-risk children. And sometimes, pediatric offices don’t share referral information (including screening results) with EI agencies. However, if the child lives in a community with systemwide care coordination, then more than 80% of referred children will be linked to the EI intervention agency or an alternative resource like Early Head Start, a parenting program, or a home visitation program. Connecticut has more than double the EI enrollment rate (3.8%) of Georgia (1.5%), even though they share the exact same eligibility definition. The difference is Connecticut’s Help Me Grow program. Nevertheless, most states lack systemwide care coordination.
Comprehensive, equitable, and tiered assessments
Nonsensically, there are 22 state-specific numerical definitions for EI eligibility, and the majority of states have inappropriately strict criteria (Pediatrics 2013 Jan:131[1]38-46). The proportion of children enrolled in EI ranges from a shameful 1.5% (Georgia) to a meager 7% (Massachusetts). On average, approximately 2.8% of children receive EI even though 25% of moderate- to high-income and 48% of low-income kindergarteners are “not ready to learn.”
Instead of a state-specific EI-eligible versus EI-ineligible process, comprehensive and equitable assessments should lead to a tiered spectrum of high-quality interventions for all at-risk children – most especially, disadvantaged children who are frequently missed. For example, the infant with a poor depressed mother is frequently deemed “ineligible,” but then is significantly behind by kindergarten age. To avoid squandering time-sensitive windows of opportunity, states need a national, research-driven definition of what constitutes a developmental–behavioral delay or at-risk condition. Families need EI or supports that are appropriately intensive, based on their continuum of need.