The resident then evaluated a random sample of notes written by each physician for diabetes or same-day appointments in the pre-scribe and scribe periods. Word counts for the entire note were measured. The notes used to establish the reliability of the ratings were excluded from the analysis for this study.
Data analysis
We used linear mixed-effects models to examine note quality measures by adjusting for possible correlations of notes from the same physician. Least-squares estimates were derived; the results were not adjusted for multiple comparisons.
RESULTS
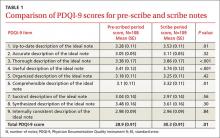
One hundred eight notes from the pre-scribe period and 109 notes from the scribe period were reviewed. Compared with notes written by a physician alone, scribed notes were rated slightly higher in overall quality (mean total PDQI-9 score 30.3 for scribe notes vs 28.9 for pre-scribe notes; P=.01) and more up-to-date, thorough, useful, and comprehensible (TABLES 1 AND 2). The differences were limited to diabetes encounters. For same day appointments, scribed notes did not differ in quality from nonscribed notes (TABLE 2). Total word count did not vary significantly between all scribe and pre-scribe notes (mean words 618, SD 273 for scribed notes vs 558 words, SD 289 for nonscribed notes; P=.12).
DISCUSSION
In this retrospective review of ambulatory notes, progress notes written by medical assistant scribes were of higher quality than notes physicians wrote alone, at least for diabetes visits. Scribe and pre-scribe notes were of similar quality for problem-focused same-day visits. This is the first study of which we are aware that compares the quality of scribed notes with notes written by physicians.
Quality scribe notes can save physician time. The progress note is an important vehicle for describing care provided and transferring information among physicians caring for the same patient. Writing a note, however, adds a considerable amount of time to the physician’s workflow. Using a scribe can decrease the time burden of note writing, and if scribed notes are of similar or better quality, this practice innovation can allow the physician to focus more on clinical than clerical tasks.
Over-documentation is a possible concern. While implementation of the EMR may improve certain aspects of quality of care delivered14,15 and note quality,16 concern has been raised about over-documentation related to the connection between documentation and reimbursement.17 In our study, we found that physician notes and scribed notes for both diabetes and same-day encounters often used EMR-based note templates, which can lead to over-documentation.
In general, both physician and scribed notes were rated to be of average to low quality because none of the mean scores on the 9 individual components of the PDQI-9 reached 4.0. Scribed notes were not inaccurate and had word counts similar to physician notes.
Scribing has potential drawbacks—and benefits. Drawbacks to scribing have not been well-studied. It has been suggested that using scribes to work around the EMR may actually hinder its further advancement because scribing insulates physicians from the inefficiencies of current EMRs and will not spur demands for improvements.3 Inaccurate or poor-quality notes could represent another downside to scribing, although concern about the quality of notes has not been documented. Our results suggest the opposite may be true.
Note quality has not been associated with quality of care as assessed by clinical quality scores,13 but using scribes may improve the quality of care in other ways. For example, the EMR may negatively affect patient-physician communication,18,19 and freeing the physician from documentation may improve the interaction.8,20 Incorporating scribing into practice may also improve the physician experience,9,10,21,22 a possible benefit that we did not measure.
We also did not measure the cost of using a scribe to assist in EMR documentation compared with the cost of physician time spent in performing this task. If the scribe model were associated with cost savings through increased physician productivity, as well as improved physician experience, future EMR development might best focus on planned utilization by physician-scribe teams.
Study limitations. The study was conducted in a single health system, although at 8 different practice sites. The sites all used the same EMR, but templates used for documentation could be individualized by the physician and medical assistant team, so our findings may reflect variation in template design. Our analysis did adjust for possible correlations of notes from the same physician. The selection of note types in our study may make our results less generalizable to other encounter types. Our sample was not large enough to detect variations in note quality among different providers and scribes.