DURBAN, SOUTH AFRICA – The first-ever nationally representative survey on sexual identity and behaviors in U.S. male high school students has exposed a high prevalence of illicit injected drug use among those who have sex with males or with both males and females.
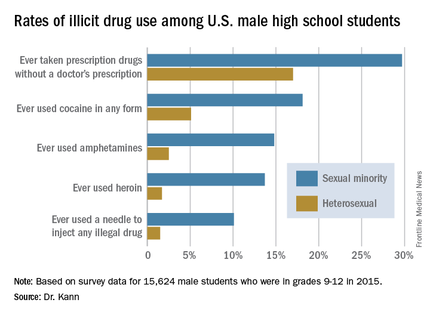
About 10% of high school boys who identify as gay or bisexual reported having ever used a needle to inject any illegal drug into their bodies, compared with 1.5% of high school boys who identify as heterosexual.
“This is a cause for great concern because of the efficiency with which injected drug use transmits not only HIV but hepatitis and other diseases,” Laura Kann, PhD, said in reporting the results of the 2015 National Youth Risk Behavior Survey (YRBS) at the 21st International AIDS Conference.
Dr. Kann of the Centers for Disease Control and Prevention’s division of adolescent and school health directs the YRBS, an annual, multiple-choice, anonymous voluntary survey that addresses six areas of risk: behaviors that contribute to unintentional injuries and violence, tobacco use, alcohol and other drug use, sexual behaviors, inadequate physical activity, and unhealthy diet behaviors.
The 2015 survey was the first ever to include questions regarding sexual identity and behaviors.
“Twenty-two percent of all new HIV diagnoses in the U.S. occur in 13- to 24-year-olds. Most occur in males who have sex with males. This makes young males an important focus for HIV prevention efforts,” Dr. Kann said.
Yet until the 2015 YRBS, no reliable estimates existed regarding the number of gay or bisexual male high school students. “Reducing HIV infection among young sexual minority males is key to reducing HIV infection in the U.S.,” she said. “It’s hard to respond appropriately to a population that has not been counted.”
The 15,624 male students in public and private school grades 9-12 who participated in the YRBS were demographically representative of the nation’s roughly 8 million male high schoolers.
About 2% of male students identified themselves as gay, another 2.4% declared themselves bisexual, 93.1% said they were heterosexual, and 2.6% were unsure. With regard to sexual behaviors, 53.3% of respondents indicated they had sexual contact with females only, 1.3% with males only, and 1.9% with both males and females; 43.6% reported they hadn’t ever had sexual contact. Respondents could interpret “sexual contact” as they wished, ranging from kissing and hugging to intercourse.
Large differences in illicit drug use behaviors were found between the sexual minorities – that is, males who had sexual contact with males or with females as well as males – and those with only heterosexual contacts.
“We need to conduct new research on injected drug use among young males who have sex with males and determine what can be done to minimize, if not eliminate, this very high-risk behavior that is occurring at alarming rates,” Dr. Kann said.
The sexual minority students were also more likely to have engaged in various forms of noninjected illicit drug use known to boost the risk of HIV infection indirectly by increasing the likelihood of having unsafe sex. The sexual minority males had significantly higher rates of having ever used cocaine in any form, of having ever used amphetamines, and of having taken prescription drugs without a physician’s prescription. For instance, 14.8% of sexual minority males reported ever using amphetamines, compared with 2.5% of heterosexual males surveyed.
She noted that the YRBS results provided no evidence that the disparity in HIV diagnoses between young males who have sex with males and young males who have sex with females are caused by differences in the prevalence of HIV-related sexual behaviors. There were no statistically significant differences between heterosexual and sexual minority students in rates of ever having had sexual intercourse, having had intercourse with four or more persons, having sexual activity currently, or having used a condom at last intercourse.
Dr. Kann called for more research in the neglected area of social issues affecting young sexual minority males that likely increase their sense of marginalization and may promote behaviors placing them at increased risk for HIV acquisition.
“Many young males who have sex with males suffer from social isolation, stress from self-concealment and from coming out, discrimination, and even hatred, which may occur at home, at school, and in communities among both their peers and the adults responsible for their care and protection,” she said. “These factors may lead to harmful coping behaviors, such as drug use, that can further increase risk for HIV infection. It’s hard to imagine how even the best intervention technology will be able to eliminate the disparities in HIV diagnosis unless these social issues are addressed first and foremost.”