Interferon-free direct-acting antiviral (DAA) regimens for chronic hepatitis C virus (HCV) infection can cause reactivation of herpesvirus, said the authors of a multicenter case series published in the November issue of Clinical Gastroenterology and Hepatology.
Reactivation occurred in 10 of 576 (2%) patients treated at three hospitals in Spain, reported Dr. Christie Perello of Puerta de Hierro University Hospital in Madrid, together with her associates. Clinicians who treat HCV should maintain a high degree of clinical suspicion for latent herpesvirus infection, particularly when patients are older or have undergone liver transplantation, and should consider varicella zoster virus vaccination before beginning DAA therapy in nontransplant patients, they said.
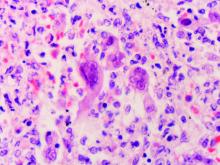
In all, 2% of patients had herpesvirus reactivations a median of 8 weeks after starting an interferon-free DAA regimen. Seven patients had cirrhosis, three were liver transplant recipients, and all achieved a sustained viral response. Seven patients were receiving sofosbuvir with ledipasvir, either with or without ribavirin; two patients were receiving ombitasvir with paritaprevir and ritonavir plus dasabuvir, with or without ribavirin; and one patient was receiving sofosbuvir with simeprevir plus ribavirin. Median age was 67 years. Seven cases involved cutaneous herpes, two involved ocular herpes, and one was herpes labialis. Two patients developed postherpetic neuralgia requiring gabapentin or pregabalin therapy, and one developed keratouveitis that was treated with valacyclovir (1 g every 8 hours for 7 days). Two other patients also received valacyclovir, three received famciclovir, and the remaining four received acyclovir. When the study was published, one patient, a 68-year-old male with postherpetic neuralgia, had residual symptoms even after undergoing antiviral therapy and nerve ablation. This patient was a liver transplantee and therefore was immunosuppressed, but like the others, he only developed herpesvirus reactivation after starting DAA HCV treatment, the researcher said.
In contrast, there were no reactivations among historical controls during a median of 37 months of follow-up. “Even when a causal relationship is not definitive, based on the temporal association and recent experience we conclude that the incidence of herpesvirus reactivation may be increased among patients on interferon-free regimens,” the researchers concluded. “More research is necessary in this new field because unexpected events might be arising in patients treated with direct-acting antivirals.”
The investigators did not report funding sources. Dr. Perello had no disclosures. Four coinvestigators reported ties to Gilead, Bristol-Myers Squibb, AbbVie, Merck Sharp & Dohme, and Janssen.