ZMapp, a potential monoclonal antibody treatment for Ebola virus disease, did not meet its efficacy goal in a clinical trial of patients in Liberia, Sierra Leone, and Guinea, according to a report in the New England Journal of Medicine.
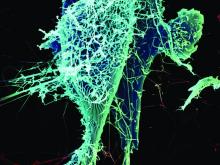
ZMapp, developed by Mapp Biopharmaceutical, comprises three different laboratory-generated monoclonal antibodies. The drug targets the main surface protein of the Ebola virus. Earlier studies in nonhuman primates demonstrated that ZMapp had strong antiviral activity and prevented death when administered as late as 5 days after experimental infection with the Zaire Ebola virus strain.
The process of ZMapp infusion was generally safe, with only one serious adverse event – hypertension – attributed to the infusion itself. Of the 93 infusions attempted in the ZMapp group, 8 were stopped because of adverse events, and 9 were slowed down to accommodate for side effects.
While ZMapp did not meet its goal, the relative risk of death was 40% lower in the ZMapp group then in the control group. Treatment with ZMapp was delayed for a week after patients became symptomatic, exceeding the 5-day window where ZMapp has been shown to have at least 90% effectiveness. In addition, of the eight patients who died in the ZMapp group, seven died before the second of the three planned ZMapp infusions were delivered.
The abrupt end to the Ebola epidemic prevented the ZMapp trial from being adequately completed. A goal of 100 patients in both groups was desired but could not be reached.
“Despite the concerted efforts of many dedicated researchers domestically and internationally who participated in this and other trials, the outbreak appears to have ended with no incontrovertible evidence that any single treatment intervention, or combination of interventions, was unequivocally superior to the types of supportive medical care typically provided,” the investigators said.
Find the full study in the New England Journal of Medicine (doi: 10.1056/NEJMoa1604330).