SAN FRANCISCO – As researchers have learned more about otitis media in the past decade, the guidelines have shifted accordingly for one of the most common conditions of childhood.
Yet some controversies remain, and the condition remains a challenge to properly identify, David Conrad, MD, of the University of California, San Francisco, said at the annual meeting of the American Academy of Pediatrics.
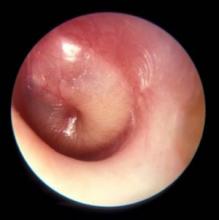
“Otitis media is really difficult to diagnose – it really is,” Dr. Conrad said. “The most important and tricky part is to distinguish otitis media from otitis media with effusion. Really, the bulging tympanic membrane is the key.” In addition, otitis media with effusion usually comes with poor balance and continued hearing loss, which the parent often picks up on.Pediatricians already know it’s the most common reason young children come into their offices and the most common reason they prescribe antibiotics. But they may know less about recognizing complications and long-term effects.
Complications and treatment
Ossicular erosion or tympanic membrane perforation are two complications; the latter’s rate is 5%-29% for untreated acute otitis media. It typically closes within hours to days, however, with a 95% closure rate within 4 weeks.
“The ear drum is pretty forgiving, pretty resilient, really,” Dr. Conrad said. The perforation occurs when pressure builds up and takes the path of least resistance through the drum, but that release of pressure also typically relieves the pain.
“Mastoiditis is one of the most feared complications, obviously,” Dr. Conrad noted, and it’s a clinical diagnosis that’s important to distinguish from mastoid effusion.
“Any child who has acute otitis media, and the middle ear fills up with fluid, which is under pressure, it will then migrate up the mastoid cavity; so, if you have an ear infection, you will have mastoid fluid – but that doesn’t necessarily mean you have mastoiditis,” he explained. “Mastoiditis is a very aggressive inflammatory process that destroys bone in the mastoid cavity. It’s often due to strep, and it’s usually a pyogenic organism that’s particularly virulent.”
Pus will then leak out from the mastoid cavity and form an abscess. If there is bone destruction, that is mastoiditis, which is treated with an ear tube or sometimes a mastoidectomy, in which a drill drains all the pus and other tissue.
Speech development and other controversies
Aside from the child’s pain, parental anxiety, and the other potential complications, researchers have learned more recently about speech delay with otitis media. The average child with recurrent otitis media or with otitis media with effusion will experience decreased hearing for about 3 or 4 months, which can affect speech, educational, and cognitive outcomes.
“If that process repeats itself, they could lose out on an entire year of not hearing well. It’s like walking around with an ear plug in,” Dr. Conrad said. It’s about a 25-35 dB hearing loss, he said, which can lead to trouble with speech discrimination, particularly with background noise, and can interfere with relationships with family, peers, and other adults.
Emerging data suggest educational difficulties, such as problems with reading comprehension, could result, and research is pivoting to look at potential cognitive development concerns, Dr. Conrad said.
“It has been noted that earlier onset of otitis media has a greater impact on educational and attention outcomes,” he said. Central auditory processing drives the development of the auditory cortex, and if that is impaired during a critical window of opportunity while synapses are forming, it could also have effects on speech.
“Otitis media and speech development is an area of controversy,” Dr. Conrad explained. Otitis media has been found to impact auditory processing skills, speech discrimination, auditory pattern recognition, and auditory temporal processing, “but there’s little evidence to support long-term language impairment,” he said.
But that’s being challenged now. Research in rats and cats in particular, however, has shown changes in the auditory cortex from ear infections.
“Most of the data are from animal models, and I think that will morph into more studies into educational outcomes in children who had a lot of ear infections when they were younger,” Dr. Conrad predicted.
Other areas of controversy relate to whether the use of the pneumococcal conjugate vaccine (PCV13), which has reduced ear infections, may have led to the rise of infections from Haemophilus influenzae and Moraxella catarrhalis, and what the duration of therapy should be for antibiotics.
If not doing watchful waiting, first-line treatment is amoxicillin or amoxicillin-clavulanate unless the child has a penicillin allergy, in which case cefdinir, cefuroxime, or cefpodoxime can be prescribed. After 48-72 hours of failed therapy, amoxicillin-clavulanate can be considered, or clindamycin or ceftriaxone, “obviously a popular option if the child has had multiple ear infections in the past month or so,” he said.
“If the child is older, we don’t treat as long,” Dr. Conrad noted. Current guidelines recommend a 10-day course if the infection resulted from strep, a 7-day or 10-day course in children aged 2-5 years, and a 5-7 day course for children older than 6 years.
Dr. Conrad reported no disclosures.