Based on the patient’s clinical presentation, he was given a diagnosis of herpes zoster oticus—also known as Ramsay Hunt syndrome. Patients with Ramsay Hunt syndrome typically develop unilateral facial paralysis and erythematous vesicles that appear ipsilaterally on the ear and/or in the mouth. This syndrome is a rare complication of herpes zoster that occurs when latent varicella zoster virus (VZV) infection reactivates and spreads to affect the geniculate ganglion.
An estimated 5 out of every 100,000 people develop Ramsay Hunt syndrome each year in the United States; men and women are equally affected. Any patient who’s had VZV infection runs the risk of developing Ramsay Hunt syndrome, but it most often develops in individuals older than age 60.
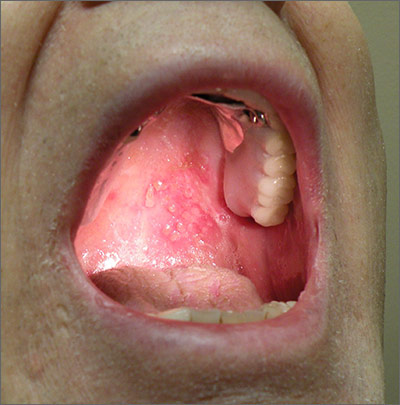
Vesicles in the mouth usually develop on the tongue or hard palate. Other symptoms may include tinnitus, hearing loss, nausea, vomiting, vertigo, and nystagmus. Because the symptoms of Ramsay Hunt syndrome suggest a possible infection, the differential diagnosis should include herpes simplex virus type 1, Epstein-Barr virus, group A Streptococcus, and measles.
A diagnosis of Ramsay Hunt syndrome is typically made clinically, but can be confirmed with direct fluorescent antibody (DFA) analysis, polymerase chain reaction (PCR) testing, or viral culture of vesicular exudates. DFA for VZV has an 87% sensitivity. PCR has a higher sensitivity (92%), is widely available, and is the diagnostic test of choice, according to the Centers for Disease Control and Prevention.
Treatment with an oral steroid, such as prednisone, in addition to an antiviral such as acyclovir or valacyclovir, may reduce the likelihood of postherpetic neuralgia and improve facial motor function. However, these benefits have not been demonstrated in randomized controlled trials.
In this case, the FP prescribed oral valacyclovir 1 g 3 times a day for 7 days and oral prednisone 50 mg/d for 5 days for the patient. After one week of treatment, the patient’s symptoms resolved and the vesicles in his mouth crusted over. He did not experience postherpetic neuralgia or have a recurrence.
Adapted from: Moss DA, Crawford P. Sore throat and left ear pain. J Fam Pract. 2015;64:117-119.