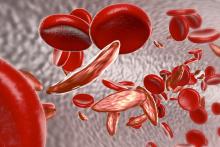
A teenage boy with sickle cell disease has been successfully treated with a therapy that uses a viral vector to insert functional genes into blood-producing stem cells.
The patient’s positive response to the intervention was first reported in 2015, and his clinical remission was reported in late 2016 at the American Society of Hematology’s annual meeting.
The new report, published online March 1 in the New England Journal of Medicine, contains the first detailed description of the case (2017;376:848-55).
The patient, who was 13 years old at the time of treatment in 2014, had the beta(S)/beta(S) genotype and severe sickle cell disease (SCD) symptoms for nearly a decade. He had been receiving prophylactic red cell transfusions for 4 years when he became the first SCD patient enrolled in HGB-205, a single-site, open-label study in France that also enrolled patients with transfusion-dependent beta-thalassemia.Treatment consisted of LentiGlobin BB305, an engineered lentiviral vector–mediated addition of an antisickling human beta-globin gene (HbAT87Q ) into the patient’s hematopoietic stem cells. The technology was developed by bluebird bio, which partially funded the study and helped design its protocol.
The investigators, led by Marina Cavazzana, MD, PhD, of Necker Children’s Hospital, Assistance Publique–Hôpitaux de Paris, collected blood-producing stem cells from the patient’s bone marrow. The cells were transduced ex vivo using LentiGlobin BB305.
After the patient underwent 4 days of myeloablation and a 2-day washout period, the transduced stem cells were infused at 5.6x106 CD34+ cells per kilogram. The patient continued receiving red blood cell transfusions until at least 30% healthy hemoglobin with the signature of the introduced gene could be detected.
Neutrophil engraftment occurred at 38 days after transplantation, and platelet engraftment, at 3 months. Red cell transfusions were discontinued at 3 months.
The patient saw vector-bearing healthy cells in the blood increase during the first 3 months after transplantation, the investigators reported, and the cells continue to be produced at stable levels through month 15, which suggests “engraftment of transduced stem cells that were capable of long-term repopulation,” the investigators wrote.
Also at 15 months after transplantation, the patient had 48% HbAT87Q, while 30% healthy hemoglobin is considered sufficient to see clinical improvement in SCD patients.
The patient has not experienced sickle cell disease–related clinical events or hospitalization since transplantation, Dr. Cavazzana and her colleagues reported, noting all his medications, including pain medication, have been stopped.
Most adverse events seen in the study were associated with busulfan, the drug used in myeloablation, and no adverse events were associated with the gene therapy itself.
These results, the investigators concluded, provide proof of concept for lentiviral vectors in delivering this gene therapy for SCD. This approach, they said, “may help to guide the design of future clinical trials of gene therapy for sickle cell disease.” One important advantage for lentiviral vectors over retroviral vectors is that the former appear less likely to generate cancer-causing mutations; the engineered vector used in this study is self-inactivating.
Two more SCD patients have since been enrolled in the same study.
In a press statement accompanying the March 1 publication, the makers of the gene therapy said these results had prompted them to modify protocols in an ongoing U.S-based study of the same therapy in SCD, in the hope of achieving outcomes similar to those seen in France.
The study was funded by bluebird bio and grants from Assistance Publique–Hôpitaux de Paris and INSERM. Of the 27 authors, 9 disclosed being stockholders of bluebird, receiving fees, holding patents on technologies used in the study, or being employees. One reported financial relationships with other firms, and 17, including the corresponding author, reported no commercial conflicts of interest.