A majority of Chikungunya infections can cause arthritis and arthralgia months or years after the initial infection, based on data from a prospective study of 307 patients.
“The most common symptoms of Chikungunya virus infection are fever associated with rheumatic manifestations,” wrote rheumatologist Eric Bouquillard, MD, of Saint-Pierre, Reunion, France, and his colleagues.
Previous studies have shown that Chikungunya virus infection is frequently the cause of joint manifestations several months or even several years after the initial infection. Following a Chikungunya epidemic on Reunion Island in 2005 and 2006, researchers enrolled 307 consecutive adults with pain secondary to Chikungunya virus infection to assess progression of rheumatic disease, including 122 (40%) with serologically confirmed infection. The average age of the patients in the study (known as RHUMATOCHIK) at baseline was 54 years, and 83% were women (Joint Bone Spine 2017 Feb 24. doi: 10.1016/j.jbspin.2017.01.014).Overall, 83% of the patients showed persistent joint pain after an average of 32 months. In addition, synovitis occurred in 64% of the patients who experienced chronic joint pain, mainly in the wrists, fingers, and ankles.
At baseline, the average number of painful joints was 6.5. At follow-up, the average number of painful joints was 3.3, and 43% of patients reported persistence of one or more swollen joints.
However, the patients reported little functional impairment; the average Health Assessment Questionnaire score was 0.44.
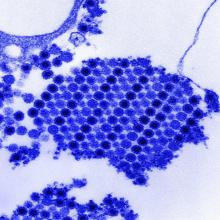
“RT-PCR [reverse transcription–polymerase chain reaction] was used in an attempt to detect the viral genome in synovial fluid samples from 10 patients, including 2 patients in the viremic phase, but the results were always negative,” the researchers noted.
Dr. Bouquillard and his colleagues enrolled the patients during April 2005-December 2006. Rheumatologic exams were conducted at baseline, and follow-up data were collected by phone surveys at 1 and 2 years after the onset of Chikungunya infection. Phone surveys were conducted by the Reunion Island Clinical Investigation Centre for Clinical Epidemiology, and interviewers also assessed patients for signs of anxiety, depression, and weakness.
The study was not designed to address treatment, but data from previous studies suggest that combination disease-modifying antirheumatic drug therapy may be more effective than hydroxychloroquine monotherapy for chronic joint pain post Chikungunya, the researchers noted.
The researchers had no financial conflicts to disclose. The study was supported in part by the Union Régionale des Médecins Libéraux de La Réunion.