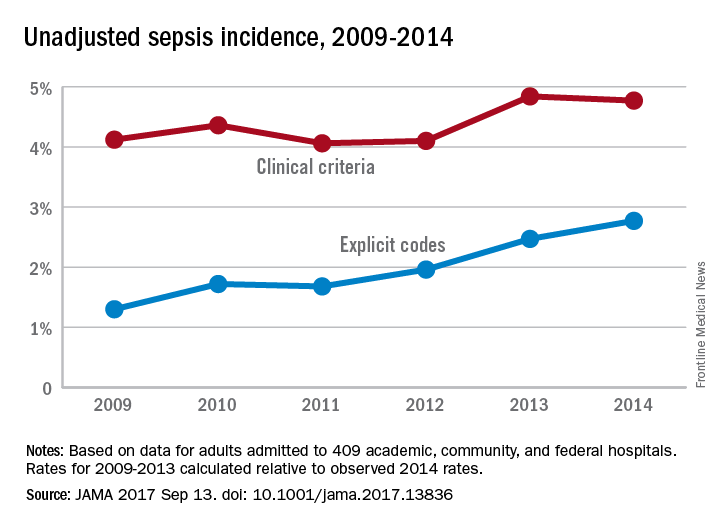
The trend for sepsis incidence from 2009 to 2014, “calculated relative to the observed 2014 rates,” was a stable increase of 0.6% per year using the more accurate of two forms of analysis, investigators reported.
The incidence of sepsis was an adjusted 5.9% among hospitalized adults in 2014, with in-hospital mortality of 15%, according to a retrospective cohort study published online Sept. 13 in JAMA.
“Most studies [of sepsis incidence] have used claims data, but increasing clinical awareness, changes in diagnosis and coding practices, and variable definitions have led to uncertainty about the accuracy of reported trends,” wrote Chanu Rhee, MD, of Harvard Medical School, Boston, and his associates (JAMA. 2017 Sep 13. doi: 10.1001/jama.2017.13836).
They used two methods – one involving claims-based estimates using ICD-9-CM codes and the other based on clinical data from electronic health records (EHRs) – to analyze data for more than 2.9 million adults admitted to 409 U.S. academic, community, and federal acute-care hospitals in 2014. The claims-based “explicit-codes” approach used discharge diagnoses of severe sepsis (995.92) or septic shock (785.52), while the EHR-based, clinical-criteria method included blood cultures, antibiotics, and concurrent organ dysfunction with or without the criterion of a lactate level of 2.0 mmol/L or greater, the investigators said.
The explicit-codes approach produced an increase of 10.3% per year in sepsis incidence from 2009 to 2014, compared with 0.6% per year for the clinical-criteria approach, while in-hospital mortality declined by 7% a year using explicit codes and 3.3% using clinical criteria, Dr. Rhee and his associates reported.
“EHR-based criteria were more sensitive than explicit sepsis codes on medical record review, with comparable [positive predictive value]; EHR-based criteria had similar sensitivity to implicit or explicit codes combined but higher [positive predictive value],” they said.
The estimates provided by Dr. Rhee and his associates provide “a clearer understanding of trends in the incidence and mortality of sepsis in the United States but also a better understanding of the challenges in improving ICD coding to accurately document the global burden of sepsis,” Kristina E. Rudd, MD, of the University of Washington, Seattle, and her associates said in an editorial (JAMA 2017 Sep 13. doi: 10.1001/jama.2017.13697).
The study was funded by the Centers for Disease Control and Prevention, Agency for Healthcare Research and Quality, National Institutes of Health, Department of Veterans Affairs, National Institutes of Health Clinical Center, and National Institute of Allergy and Infectious Diseases. Three of Dr. Rhee’s associates reported receiving personal fees from private companies or serving on advisory boards or as consultants. No other authors reported disclosures. Dr. Rudd and her associates had no conflicts of interest to report.