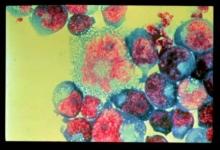
Higher frequency of alpha4beta7 expression in the CD4 T cells in the gut was associated with increased HIV acquisition and severity, according to the results of a retrospective comparative analysis of blood samples from patients in the CAPRISA 004 study.
Researchers compared samples from patients who eventually developed HIV with samples from those who did not; they also assessed human study cohorts from Kenya and the RV254/Search 010 cohort in Thailand, according to an online report in Science Translational Medicine. In addition, they obtained data from nonhuman primates (NHPs) challenged with simian immunodeficiency virus (SIV) to compare results between primate species.
They found that alpha4beta7+ CD4+ T cells were depleted very early in HIV infection, particularly in the gut, and the initiation of antiretroviral therapy (ART) was unable to restore the normal levels of those cells even when provided at the earliest time point. Citing the literature, the researchers speculated that interactions between alpha4beta7 and the HIV env protein may assist the virus in locating its ideal target cells, and that high levels of alpha4beta7+ CD4+ T cells were associated with preferential infection by HIV-1 types containing motifs associated with higher alpha4beta7 binding, which are overrepresented in the region where the CAPRISA004 study was conducted.
“Although the association of alpha4beta7 and HIV expression was relatively modest, results were consistent in independent cohorts in two different countries and in NHPs,” according to Aida Sivro, PhD, of the Centre for the AIDS Programme of Research and her colleagues on behalf of the CAPRISA004 and RS254 study groups.
NHP studies showed some promise in this regard because, while ART alone did not lead to immune restoration of these T cells, “ART in combination with anti-alpha4beta7 did so in NHPs,” the researchers concluded, suggesting the possibility of additional therapeutic interventions in humans.
The authors reported having no disclosures. The CAPRISA 004 study was funded by the U.S. National Institutes of Health, U.S. Agency for International Development, and the South African Department of Science and Technology.
SOURCE: Sivro A et al. Sci Transl Med. 2018 Jan 24;10(425):eaam6354.