Chikungunya infections in young children resemble skin symptoms characteristic of Stevens-Johnson syndrome and toxic epidermal necrolysis, (SJS-TEN), according to data from a case series of 21 children seen during a chikungunya outbreak in India in August and September 2016.
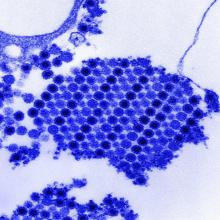
“Cutaneous involvement in chikungunya is seen in 40%-75% of patients,” having varied presentations, wrote Taru Garg, MD, and colleagues at the Lady Hardinge Medical College and Associated Hospitals, New Delhi, India. Chikungunya mimicking SJS-TEN is rare: 96 cases have been reported in the literature, to the investigators’ knowledge.The researchers described their observations of 13 boys and eight girls aged 1-36 months in Pediatric Dermatology. All 21 children presented with vesiculobullous and necrotic lesions and mild to moderate fever; 16 children (76%) had large erosions, purpuric macules, and necrosis. Most of the lesions occurred on the extremities.
The time from the onset of illness to presentation ranged from 1 to 9 days, and the skin lesions resolved in 5-7 days. The lesions resolved with no sequelae in 11 patients, with hyperpigmentation in seven (33%) , and with hypopigmentation in three patients (14%).
In addition, three patients (14%) developed minor oral erosions, and four (19%) developed palmoplantar erythema, which also may be associated with SJS-TEN. However, none of the patients experienced the severe mucositis and ocular and genital involvement common to SJS-TEN, Dr. Garg and associates noted. A total of seven children tested positive for chikungunya based on enzyme-linked immunosorbent assay results.
Severity of illness can be helpful to distinguish chikungunya from SJS-TEN, the researchers said. Based on the Nelson severity index, 11 children in this series met the criteria for “not sick,” nine were “moderately sick,” and one was “very sick.”