Since the advent of multichannel serum chemistry screening in the 1970s, large numbers of asymptomatic cases of primary hyperparathyroidism (PHPT) have been discovered. The clinical spectrum of the disease has changed from the classic “moans, groans, bones, and stones” to an asymptomatic and subtle presentation of hypercalcemia.1,2 PHPT and malignancy are the most common causes for hypercalcemia, accounting for 90% of cases.3 In the United States, the estimated incidence of PHPT between 1998 and 2010 was about 50 per 100,000 person-years. Most patients with PHPT are older women (ages >50 years) who are asymptomatic at the time of diagnosis.1
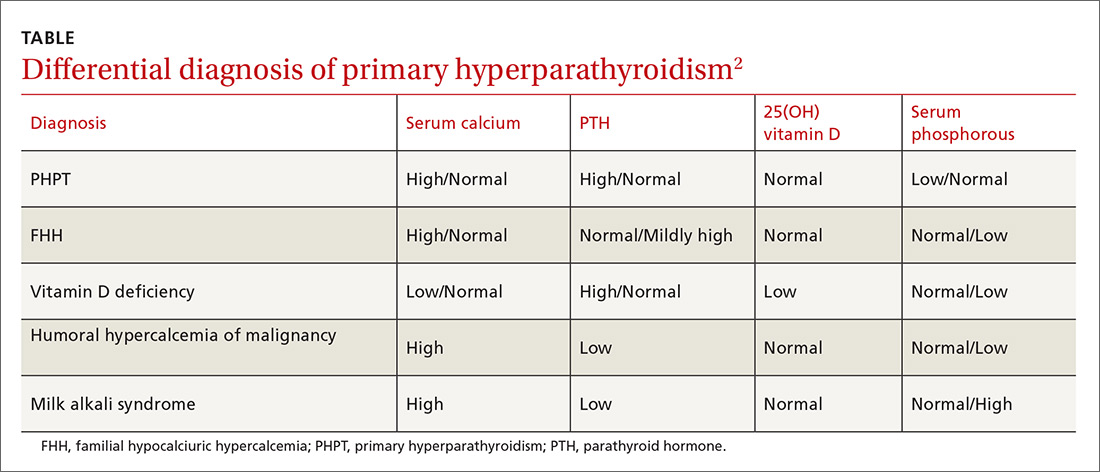
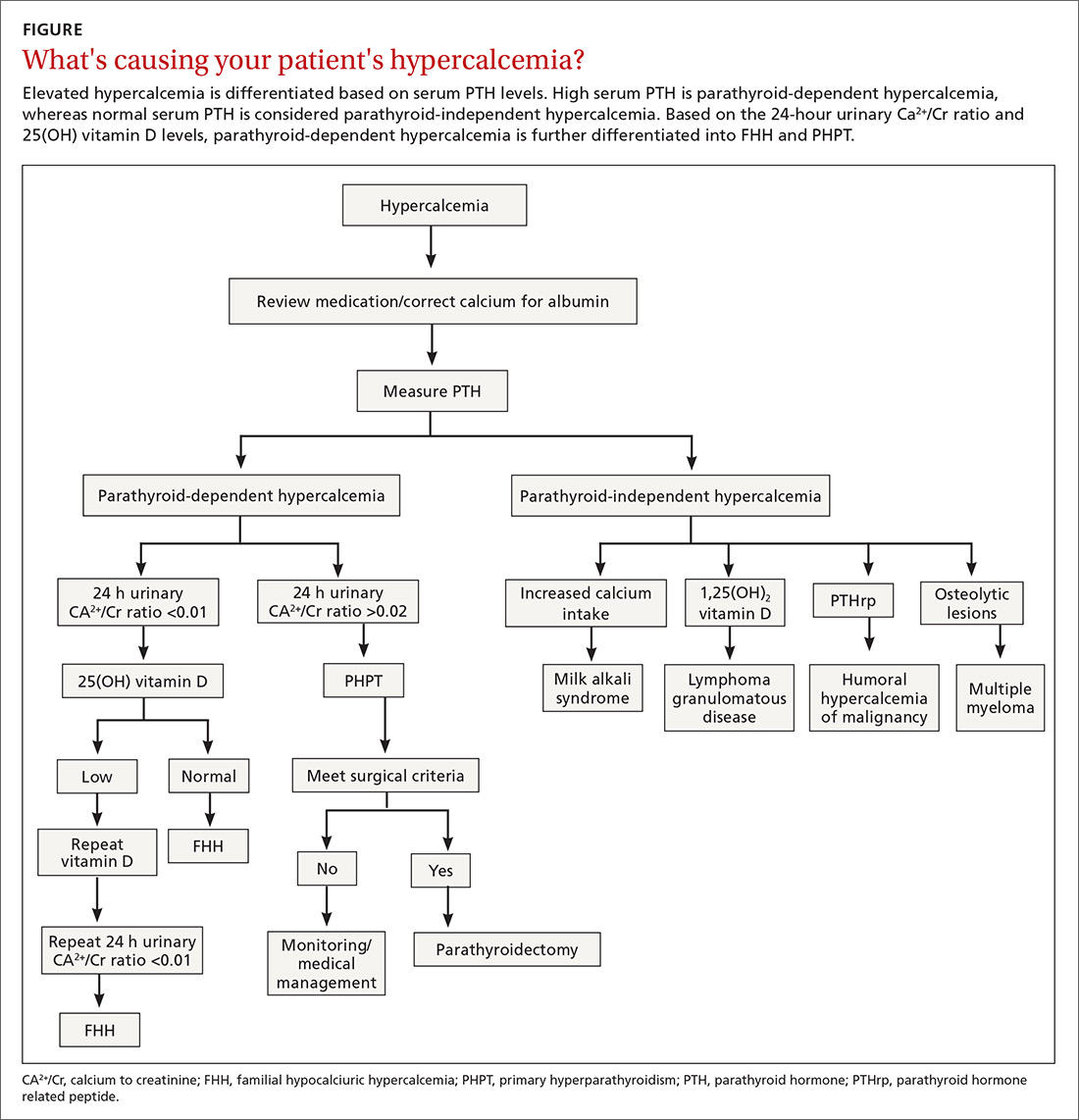
Vigilance needed in primary care. PHPT is slowly progressive, and the patient might accept symptoms as a process of aging. Therefore, it is essential that primary care physicians (PCPs) be aware of the diagnostic and management options. A systematic approach to the diagnosis of PHPT helps differentiate the causes of hypercalcemia (TABLE2; FIGURE2). But before we discuss PHPT diagnostic clues, it’s helpful to quickly review the workings of the parathyroid glands.
How the glands work, what can go wrong
Parathyroid hormone (PTH) is secreted by 4 pea-sized parathyroid glands located posterior to the thyroid. PTH regulates the levels of calcium (Ca2+) and phosphorous and controls the conversion of 25(OH) vitamin D to 1,25(OH)2 vitamin D by activating the enzyme 1 alpha-hydroxylase.
PHPT is regarded as an abnormal secretion of PTH that does not correlate with the levels of Ca2+ in the blood.1 Eighty percent of PHPT is due to a solitary adenoma in one of the parathyroid glands, 2% to 4% is secondary to multiple parathyroid adenomas, 15% is due to parathyroid hyperplasia, and 0.5% due to parathyroid carcinoma.4
Nonspecific symptomsare subtle clues of PHPT
Patients with PHPT can present with nonspecific symptoms, such as weakness, fatigue, anorexia, polyuria, polydipsia, bone and joint pain, mild depression, and mild cognitive or neuromuscular dysfunction.5 A careful history is essential to elicit these symptoms, as the patient may attribute these to aging or other causes. PHPT should also be considered when patients present with kidney stones, unexplained osteoporosis, or fragility fractures. A physical examination is seldom helpful, as parathyroid adenomas are hardly ever palpable. A slit-lamp examination may reveal corneal diseases in rare cases of hypercalcemia.6
Which lab tests, imaging should you order?
Serum Ca2+
Repeat measurements of serum Ca2+ to confirm hypercalcemia. Volume depletion, underlying malignancy, medications such as hydrochlorothiazide, lithium, and excess intake of Ca2+ carbonate can cause hypercalcemia.7 Therefore, a review of the patients’ home medications and dietary preferences in the evaluation of hypercalcemia is essential. The 2 most common causes of hypercalcemia are hyperparathyroidism and hypercalcemia of malignancy.
For hypercalcemia, establish a differential diagnosis by measuring intact PTH. An increased serum Ca2+ level along with an elevated PTH concentration should suggest PTH-dependent hypercalcemia, whereas hypercalcemia with suppressed or low-normal PTH values should suggest PTH-independent hypercalcemia (granulomatous disorders, hypercalcemia of malignancy).
Continue to: Hypercalcemia of malignancy is due to...