according to the 2018 update to U.S. guidelines for cholesterol management from the American Heart Association and the American College of Cardiology.
The guideline also emphasizes “careful adherence to lifestyle recommendations at an early age [to] reduce risk factor burden over the lifespan and decrease the need for preventive drug therapies later in life,” Scott M. Grundy, MD, PhD, and Neil J. Stone, MD, said in a synopsis of the document in the Annals of Internal Medicine.
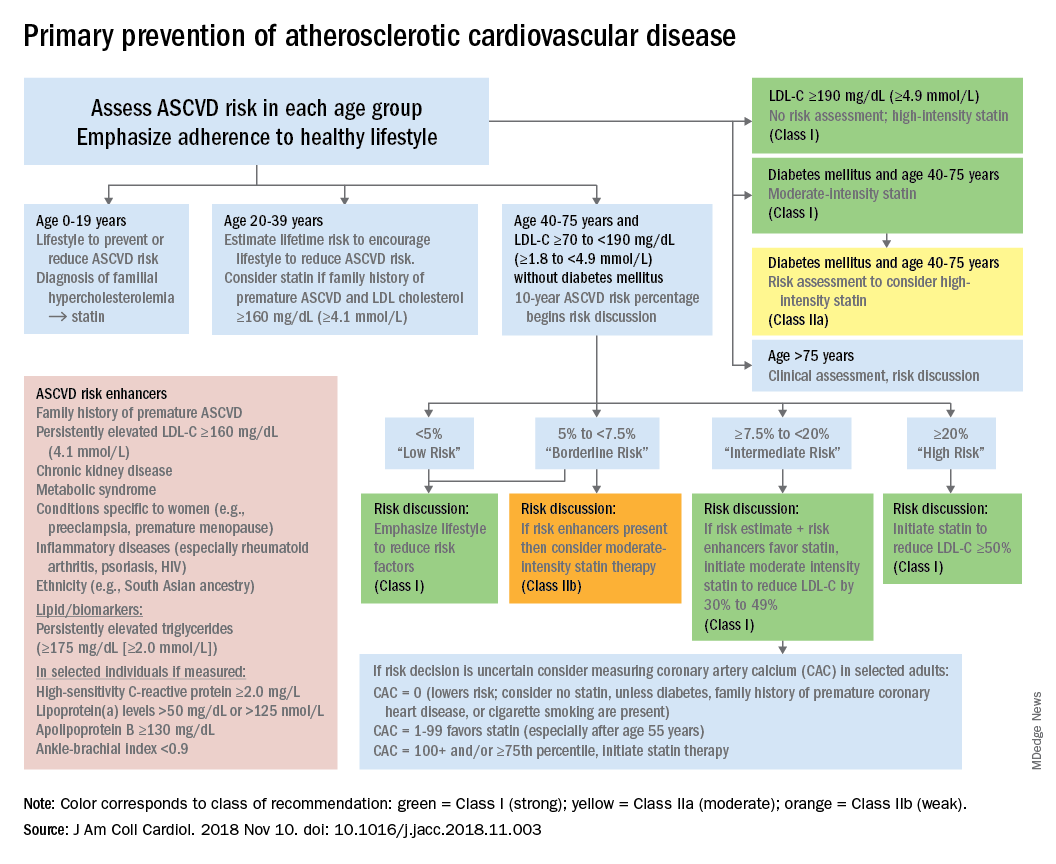
For primary prevention in patients aged 40-75 years, estimation of 10-year ASCVD risk – introduced in the 2013 guidelines – and stratification into one of four categories should set the stage for clinician-patient discussion. A score of less than 5% indicates low risk and should prompt a risk discussion that emphasizes lifestyle recommendations. “Statins are clinically efficacious in the latter three categories, but the higher the risk, the stronger the statin indication,” said Dr. Grundy of the University of Texas, Dallas, and Dr. Stone of Northwestern University, Chicago.
When risk status is uncertain, measurement of coronary artery calcium should be considered in patients aged 40-75 years with LDL cholesterol levels of 70-189 mg/dL who do no not have diabetes, they noted.
The guideline emphasizes secondary prevention with “maximally tolerated doses of statins” and the use of nonstatin drugs such as ezetimibe and PCSK9 inhibitors for patients with very high ASCVD risk – defined as a history of multiple major events or one event and other high-risk conditions, Dr. Grundy and Dr. Stone wrote.
Financial support for the Guideline Writing Committee for the 2018 Cholesterol Guidelines came from the AHA and the ACC. Dr. Grundy and Dr. Stone said that they had no relevant conflicts of interest.
SOURCE: Grundy SM and Stone NJ. Ann Intern Med. 2019 May 28. doi: 10.7326/M19-0365.