, a study has found.
“Incorrect inhaler technique cannot explain the poor disease control in our patient population,” wrote Patrick K. Gleeson, MD, of the University of Pennsylvania, Philadelphia, and coinvestigators. Their report is in the Journal of Allergy and Clinical Immunology: In Practice. “In individuals with poorly controlled asthma, other factors contributing to disease mortality must be considered.”
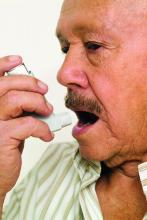
The 586 patients in the study were observed using their inhalers, and their technique was scored by way of a checklist developed for the study. Inhaler technique – widely regarded as a risk factor for poor disease control – was “better than expected,” the investigators reported, with 56% of patients using metered dose inhalers and 64% of those using dry powder inhalers not making any errors.
“The seeming disassociation between subjects’ asthma control and inhaler technique is counterintuitive, and may be explained by important baseline characteristics in our patients,” they wrote. For instance, participants had suboptimal living conditions in lower income Philadelphia neighborhoods. Almost a quarter – 23% – were current smokers, and almost half were Medicaid recipients. In addition, their mean body mass index was 35.1 kg/m2.
The investigators hypothesized that patients with lower health literacy would have poorer technique but found instead that technique did not vary by reading comprehension or numeracy levels.
More than half of the adults in the study had uncontrolled asthma as defined by prednisone use, an emergency department visit, or a hospitalization for asthma in the past 12 months. A subset had moderate to severe disease per a physician’s diagnosis, forced expiratory volume in 1 second less than 80% predicted, and improvement with a bronchodilator. All patients, however, were considered to have uncontrolled asthma.
There is “uncertainty” in the field about how to measure inhaler technique, and the technique checklist used in the study “may have omitted potentially important errors,” the investigators noted. Still, “good technique predominated among our [population of vulnerable patients].”
The project was supported through awards from the National Institutes of Health/National Heart, Lung, and Blood Institute and the Patient-Centered Outcomes Research Institute.
Coinvestigator Andrea J. Apter, MD, reported that she consults for UpToDate and is an associate editor for the journal. Coinvestigator Knashawn H. Morales, ScD, reported owning stock in Altria Group, British American Tobacco, and Philip Morris International. The other authors reported having no conflicts of interest.
SOURCE: Gleeson PK. J Allergy Clin Immunol Pract. 2019 Jun 5. doi: 10.1016/j.jaip.2019.05.048.