Roughly half of American adults have hypertension, and about 71% of these cases are uncontrolled, according to data from the American Heart Association.
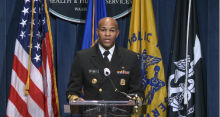
If left uncontrolled, hypertension can increase risk for conditions including heart disease, stroke, kidney disease, pregnancy complications, and cognitive decline, surgeon general Vice Adm. Jerome M. Adams, MD, said in a teleconference on Oct. 7. Hispanic and Black individuals are disproportionately affected, he added.
“We cannot wait to deal with this epidemic of uncontrolled high blood pressure,” even in the midst of the ongoing COVID-19 pandemic, said Dr. Adams. “We know what works” to help control hypertension, he added, citing his own use of a blood pressure monitoring device at home.
The Department of Health & Human Services has issued a Call to Action to Control Hypertension based on the latest science and research.
Dr. Adams outlined three goals to improve hypertension control, starting with making it a national priority. The Call to Action supports increasing awareness of the health risks associated with hypertension, recognizing the economic impact, overcoming barriers to controlling hypertension, and promoting health equity.
“In 2020, disparities in the burden of disease – especially among minority populations – have been recognized during the COVID-19 pandemic. A growing body of evidence has shown that people with underlying health conditions, including cardiovascular disease, are at increased risk of worse outcomes related to COVID-19 infection,” according to the Call to Action.
A second goal is to build and sustain communities that support individuals in taking responsibility for their health and blood pressure control, Dr. Adams said. He cited the need to create places for safe physical activity, access to healthy food, and opportunities to connect to resources to support lifestyle changes.
Finally, clinicians should continue to use standardized treatment approaches and promote team-based care to maximize outcomes for patients, Dr. Adams said.
Success starts with making hypertension control a priority across the leadership team, regardless of the size, location, or demographic population at a health care setting, he said. Dr. Adams cited the Million Hearts 2022 program, an ongoing initiative to prevent 1 million heart attacks in the United States over 5 years, as a way that HHS is recognizing and rewarding success stories in hypertension control from across the country.
Empowering patients and equipping them to take charge of their hypertension essential to reducing the epidemic of high blood pressure, especially during the ongoing pandemic, Dr. Adams said. His message to clinicians to extend to patients is that it is safe to visit their doctors. Hospitals have worked to create a safe environment, however, patients can and should monitor their blood pressure regularly at home, using a self-measured blood pressure monitoring (SMBP) device, which may be covered by some insurers.
“I would encourage people to know their numbers,” and that 130/80 mm Hg is considered high and a risk factor for poor health outcomes, Dr. Adams said. Clinicians also should continue to support patients in lifestyle changes such as healthy eating and exercising regularly to help control high blood pressure.
The AHA expressed support for the surgeon general’s Call to Action. “Today’s call to action references updated hypertension guidelines the AHA and the American College of Cardiology issued in 2017 that apply the latest science to help clinicians work with patients to control their blood pressure,” the AHA said in a statement. The AHA also called on the Centers for Medicare & Medicaid Services and other insurance providers “to include coverage of SMBP devices for treatment and management of hypertension.”
The Call to Action was accompanied by a Viewpoint from Dr. Adams and Janet S. Wright, MD, also of the HHS, published in JAMA. Dr. Adams and Dr. Wright emphasized that the timing of the Call to Action recognizes that many of the same social factors that support or impede successful high blood pressure control are factors in worse outcomes from COVID-19 infections as well.
“When coupled with widespread implementation of best practices in clinical settings and empowering individuals to actively manage their blood pressure, acknowledging and addressing a community’s social conditions may generate sustained improvements in control of both hypertension and COVID-19,” they said.
Read and download the full Call to Action here, and read the Executive Summary at hhs.gov.