ATLANTA – All health care personnel should receive a single dose of the tetanus-diphtheria-acellular pertussis vaccine if they have not already, regardless of the duration since their last tetanus-diphtheria dose.
That recommendation, approved on Feb. 23 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention, updates a previous ACIP recommendation (MMWR 2006;55:RR-17).
The committee also voted separately to recommend postexposure antimicrobial prophylaxis for all health care personnel (HCP) who have unprotected exposure to pertussis and are likely to expose high-risk patients – such as pregnant women or hospitalized newborns – to the disease, even if the HCP were previously vaccinated.
"Protecting HCP from acquiring and transmitting infectious diseases is a public health goal," said Dr. Jennifer Liang of the CDC’s National Center for Immunization and Respiratory Diseases.
In one hospital-based study of serum samples collected over 1-3 years, serologic evidence of pertussis infection was detected in 2 of 106 residents, for an annual incidence rate of 1.3%, and 3 of 39 emergency department employees, for annual incidence rate of 3.6%. Two of the five infected subjects had symptomatic disease (Infect. Control Hosp. Epidemiol. 1999;20:120-3).
The new Tdap recommendation removes a previous 2-year interval requirement since the last Td dose, and also includes HCP who are aged 65 years and older. Since Tdap is not currently licensed for multiple administrations, subsequent routine 10-year boosters should be given as Td, according to the language the committee approved by a near-unanimous vote of 14 members, with just one abstaining.
Also included was a recommendation that hospitals and ambulatory care facilities provide Tdap for HCP and use approaches that maximize vaccination rates, such as education about the benefits of vaccination, convenient access, and provision of the vaccine at no charge.
The second vote was aimed at addressing the fact that pertussis infection can occur even among those who are immunized. In an as-yet unpublished study from Vanderbilt University in Nashville, Tenn., of 116 exposures to pertussis among different HCP, pertussis infection did not occur in 40 of 44 (91%) of those who were monitored but did not receive postexposure prophylaxis (PEP) compared with 41 of 42 (98%) of those who received PEP.
While not conclusive, those findings suggested that there may be a benefit to both monitoring and PEP in vaccinated HCP, Dr. Liang said.
In addition to the PEP recommendation for HCP with unprotected exposure to pertussis who are likely to expose high-risk patients, ACIP also advised that other vaccinated HCP should either receive antimicrobial PEP or be monitored daily for 21 days after pertussis exposure and treated at the onset of signs and symptoms of pertussis.
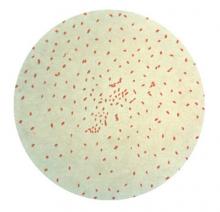
Health care facilities should maximize efforts to prevent transmission of Bordetella pertussis, and take respiratory precautions to prevent unprotected exposure to pertussis, ACIP advised.
As an employee of the CDC, Dr. Liang has no relevant financial disclosures.