Magnetic resonance imaging is an important tool for detecting subclinical arthritis in children with juvenile idiopathic arthritis. In addition, MRI is a useful way to determine if there is disease persistence or silent progression before discontinuing treatment, according to a study of children who have clinically inactive JIA or are in remission on medication, according to Dr. Nikolay Tzaribachev.
All of the patients with clinically defined persistent oligoarticular juvenile idiopathic arthritis (JIA) were found to have polyarticular disease on MRI, according to Dr. Tzaribachev, head of the pediatric rheumatology department at the Center for Rheumatic Diseases in Bad Bramstedt, Germany.
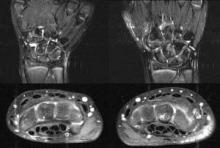 Photo credit: Courtesy Dr. Nikolay Tzaribachev
Photo credit: Courtesy Dr. Nikolay Tzaribachev
7 year old girl with clinical involvement only of the right wrist (oligoarthritis). Left side at first clinical visit, right side in a state of clinical inactivity (no symptoms, no lab abnormalities) after two months of drug treatment. On both left and right side polyarticular joint involvement on MRI.
"JIA tends to have an insidious onset and disease course. Subclinical JIA can elude the human tactile senses and clinical capacity to detect arthritis. In patients who are on drug treatment, symptoms may drop beyond clinical activity and disease may only become detectable by imaging techniques," said Dr. Tzaribachev in an interview.
"Remission criteria appear to be insufficient to detect the real extent of disease, which is of high importance to prevent joint damage, especially in growing children, who are supposed to become healthy adults.
"Furthermore, differentiation between oligo- and polyarticular disease at the first clinical evaluation after onset of symptoms is indispensable, since according to the ACR 2011 treatment guidelines [Arthritis Care Res. (Hoboken) 2011;63:465-82], oligo- and polyarticular disease have different treatment approaches," he noted.
During the last few years, silent arthritis in adults with RA has been detected only through the use of different imaging techniques, according to Dr. Tzaribachev. This fact led him and his colleagues to speculate that silent arthritis might also be the cause of the high percentage of disabilities in young adults with JIA, and that the clinical criteria for inactive disease and remission in JIA might be inadequate for detecting silent arthritis.
"We saw the huge discrepancy between clinical examination and MRI results, and understood the urgent need for more knowledge about the real extent of disease and silent disease progression, in order to protect the children from joint damage," said Dr. Tzaribachev.
The study included 21 patients with JIA (median age, 10.2 years at enrollment), who were on medications including NSAIDs, methotrexate, and/or tumor necrosis factor antagonists.
Clinically inactive disease or remission on medication were defined according to the Wallace criteria (J. Rheumatol. 2006;33:789-95). Patients underwent clinical examination, laboratory tests, and MRIs, and were asked to fill out a child health assessment questionnaire at every visit. The joints examined included wrists, knees, and ankles. Clinical and MRI exams and laboratory investigations were performed on the same day. Joint counts included those done clinically, as well as those based on MRI findings.
JIA subtype distribution included persistent oligoarticular (five patients), extended oligoarticular (four), polyarthritis (six), psoriatic arthritis (five), and undifferentiated arthritis (one). The median follow up time was 2.5 years.
Overall, 45 events were documented, 29 of which involved silent arthritis.
In all events, MRI revealed the following findings: 36 events with joint effusion, 39 with synovitis, 42 with synovial hypertrophy, 15 with bone marrow edema, 14 with osteitis, 15 with erosions, and 3 with tenosynovitis. All the silent arthritis events involved signs of arthritis that could be seen on MRI. Silent arthritis events were followed after a delay by clinical activity, according to the study.
In patients with JIA who present with clinically inactive disease or remission on medication, flares are preceded by arthritis detected on MRI. "In those cases, clinical examination and laboratory parameters remain normal despite ongoing disease activity, and remission criteria fail to show the real extent of disease," said Dr. Tzaribachev. "The lack of symptoms may also lead to silent disease progression, explaining the high percentage of physical disabilities in young adults with JIA. Imaging seems to be an important tool for defining disease activity, which should be included in the remission criteria and performed before treatment discontinuation."
The JIA classification probably needs to be redefined and remission criteria need to be reviewed to allow for the use of MRI and ultrasound, said Dr. Tzaribachev. Imaging techniques and protocols also need to be improved to become more child friendly, he noted. In addition, more studies are needed to define normal findings with respect to the growing musculoskeletal system in children and to allow for differentiation from mild pathology, especially for new imaging techniques like Xiralite. "Last, but not least, as in adult rheumatology, imaging should probably find its place in all clinical trials of children with inflammatory arthritis," he said.


