BOCA RATON, FLA. — At 1 year after surgery, laparoscopic sleeve gastrectomy is associated with morbidity and effectiveness rates between those of laparoscopic adjustable gastric band and laparoscopic Roux-en-Y bypass procedures, according to the first report from the American College of Surgeons – Bariatric Surgery Center Network accreditation program.
The ACS project collected prospective, longitudinal, standardized data from 109 hospitals for this initial report on laparoscopic sleeve gastrectomy, a newer bariatric procedure that’s being performed with increasing frequency.
"This is an observational study that reflects the cases now being done. Right now we don’t know the ideal candidates for this operation. But we can show that it’s a safe operation, it’s approved by the different societies, and it should be reimbursed by the various payers," Dr. Matthew M. Hutter said at the annual meeting of the American Surgical Association.
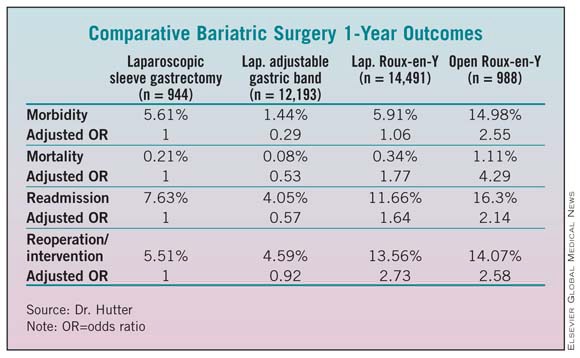
Included in the analysis were 1-year outcomes for 944 patients who had laparoscopic sleeve gastrectomy, 12,193 who underwent the laparoscopic adjustable gastric band procedure, 14,491 who had laparoscopic Roux-en-Y gastric bypass, and 988 who had an open Roux-en-Y gastric bypass. Morbidity, readmission, and reoperation/intervention rates were lowest with the gastric band procedure and highest with open Roux-en-Y. Differences in 1-year mortality did not reach statistical significance. Additional years of careful follow-up are planned, according to Dr. Hutter of Massachusetts General Hospital, Boston.
The absolute reduction in body mass index at 1 year was smallest in the laparoscopic adjustable gastric band group at about 6 kg/m2, greatest with open or laparoscopic Roux-en-Y bypass at about 15 kg/m2, and intermediate at close to 12 kg/m2 with laparoscopic sleeve gastrectomy.
Discussant Dr. Carlos A. Pellegrini called the study a landmark in surgical history.
"It captures a novel procedure as it launches into general practice, assessing both safety and effectiveness of sleeve gastrectomy at a time when case reports and case series by advocates dominate the literature," the surgeon observed. "Compare this to the introduction of laparoscopic cholecystectomy in the late ‘80s: weekend courses, no surveillance, no monitoring, common bile duct injuries hurting patients and us calling [the results] our learning curve.
"Times have changed, and surgeons should take credit for it. This study represents a milestone in the ways we think about safety, launch a new surgical intervention, and monitor its impact," said Dr. Pellegrini, professor and chairman of the department of surgery at the University of Washington, Seattle.
Although the operation appears to be safe and have a low risk profile, additional years of follow-up will be important in gauging the procedure’s effectiveness. European surgeons report that the stomach can dilate over time, which may reduce laparoscopic sleeve gastrectomy’s effectiveness, he said.
Dr. Hutter reported having no financial conflicts.