DENVER – Pediatric hospitalists adhere more closely to bronchiolitis management guidelines than do nonhospitalist pediatricians, according to a multicenter chart review.
The implication is that hospitalists therefore provide a higher quality of care. This notion is supported by the study finding that hospitalist-managed patients were less likely to be admitted to the intensive care unit. On the other hand, neither overall length of stay nor rates of rehospitalization within 4 weeks were significantly different for pediatric hospitalist- and nonhospitalist-managed patients with bronchiolitis, Dr. Russell McCulloh reported at the annual meeting of the Pediatric Academic Societies.
Prior attempts to compare the quality of care provided by pediatric hospitalists and nonhospitalists have generally relied upon self-reported rates of guideline adherence obtained in physician surveys. To generate more objective data, Dr. McCulloh and coworkers at Hasbro Children’s Hospital in Providence, R.I., analyzed the charts of 713 children with bronchiolitis who were admitted to the pediatric hospitalist and nonhospitalist pediatric services at two academic tertiary medical centers in 2007-2008.
The investigators selected bronchiolitis as the index diagnosis for their quality-of-care study because it is the No. 1 cause of hospital admission in children. The quality standard against which physician management was measured was the 2006 American Academy of Pediatrics guidelines for bronchiolitis diagnosis and management (Pediatrics 2006;118:1774-93).
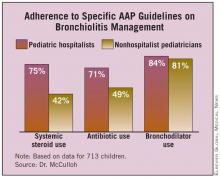
Reviewers focused on three quality indicators contained in the guidelines. First, the AAP guidelines recommend that corticosteroids shouldn’t be used routinely in the management of bronchiolitis. Pediatric hospitalists were clearly more in step with this guidance. The review showed that they discontinued systemic steroids when no indication existed 75% of the time, compared with 42% for nonhospitalists, according to Dr. McCulloh.
Second, hospitalists similarly discontinued antibiotics in the absence of specific indications of a coexistent bacterial infection 71% of the time. Nonhospitalist pediatricians were in step with this AAP recommendation only 49% of the time.
Third, regarding the discontinuation of bronchodilators in the absence of a documented, objective, positive clinical response, both types of physicians showed room for improvement. Hospitalists stopped albuterol in only 84% of cases when it had been proved ineffective; nonhospitalist pediatricians did so 81% of the time. Those rates of guideline adherence are insufficient, Dr. McCulloh commented.
On the other hand, hospitalists discontinued unneeded racemic epinephrine 93% of the time, as did nonhospitalists in 91% of cases in which it was appropriate to do so.
Rehospitalization within 4 weeks occurred in 4.6% of pediatric hospitalist–managed patients and in 7.2% of those managed by nonhospitalist pediatricians, a nonsignificant difference. In contrast, the 10.9% ICU admission rate for hospitalist-managed bronchiolitis patients was significantly lower than the 16.3% rate among children managed by nonhospitalists.
Dr. McCulloh declared having no financial conflicts.