CHICAGO – The effect of proton pump inhibitors on Clostridium difficile infection was neither strong nor consistent in a longitudinal hospital cohort of 61,834 patients.
Previously conducted case-control studies reported that PPIs were associated with a two- to threefold increase in the risk of C. difficile infection (CDI), but these latest findings suggest that the impact of PPIs may be overstated, Dr. Kyoung Sup Hong said at the annual Digestive Disease Week.
In his study, CDI incidence per 1,000 person-years was 3.5 in patients receiving PPIs for less than 3 months (group 1), 7.4 in those on PPIs for 3 months, but less than 1 year, (group 2), and 4.5 in those on PPIs for at least 1 year (group 3).
In logistic regression analysis that adjusted for PPI exposure, age, comorbid conditions, and antibiotic use in the previous 8 weeks, the association between PPI duration and CDI was significant, increasing from an odds ratio of 1 in group 1 (reference) to 2.59 in group 2 (P value less than .01), and to 2.17 in group 3 (P less than .01), Dr. Hong said.
Notably, the use of antibiotics in the previous 8 weeks significantly increased the risk of C. difficile infection to a whopping odds ratio of 31.73 (P less than .01).
In a Cox proportional hazard model that further adjusted for the interval between PPI start to CDI attack or last follow-up, however, the association between PPI use and CDI was significant only for group 2 (hazard ratio 1.94, P less than .001) and not group 3 (HR. 1.22, P = .25), said Dr. Hong of Seoul (South Korea) National University.
"We conclude that PPIs’ impact on CDI is neither strong nor consistent; therefore, PPIs seem to be an important confounder rather than a cause of CDI," he said.
A recent study among hospital discharges (Arch. Intern. Med. 2010;170:784-90) reported a dose-response effect with acid suppression and the risk of CDI, but Dr. Hong noted that it provided no information about medications before admission. In that study, the risk of CDI on or after the third hospital day increased from 0.3% in nonusers to 0.6% in those receiving histamine2 receptor antagonist therapy, to 0.9% in those receiving daily PPI therapy, and to 1.4% in those receiving more-frequent PPI therapy.
Dr. Hong and his colleagues aimed to evaluate the effect of PPI treatment duration on CDI development among all adults, older than age 20 years, who visited the Seoul National University Hospital and took a prescription PPI from January 2005 to December 2009.
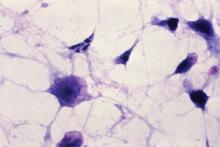
Among the 61,834 patients, there were 534 CDI cases, of which 5 were identified with endoscopy only, and the remaining 529 by a positive C. difficile toxin assay.
CDI was reported in 319 of the 50,534 (.63%) patients in group 1; 176 of the 9,122 (1.94%) patients in group 2; and 38 of the 2,178 (1.74%) patients in group 3. The average follow-up time from the first PPI prescription until the last visit was 22 months, 32 months, and 47 months, respectively.
Patients infected with C. difficile were significantly older (61 years) than those without CDI at (56 years) (P less than .01). Age remained a significant risk factor for CDI in both multivariate logistic regression (OR 1.016, P less than .001) and Cox proportional (HR 1.018, P less than .001) analyses.
Dr. Hong acknowledged that the study was limited by use of a hospital cohort, and thus the data could not be translated directly to the community.
Dr. Hong and his colleagues reported no conflicts of interest.