The decades-long shift in our approach to prenatal screening, which brought us from a point that maternal age was the main criterion for assessing risk of chromosomal abnormalities to a more precise first-trimester screening approach – one that that combines biochemistry and imaging – is continuing to evolve.
Indeed, researchers are honing in on a "platform" of first-trimester assessments that can screen for an even wider array of risks and pregnancy complications than previously envisioned – an array that extends far beyond chromosomal abnormalities. Much of this first-trimester screening platform is currently being applied and is poised to become a new standard of care.
The continued evolution of first-trimester screening is critical, as a massive amount of time and resources is spent trying to identify problem pregnancies. Many of these resources still are used inefficiently because detection is incomplete or too late to make a difference. With an expanded and precise first-trimester platform for assessment, we can offer women and their physicians significantly more information early on. This will enable us to channel our resources to improve decision making, direct management, and enhance pregnancy outcome.
Early Screening’s Development
Prenatal screening used to be all about maternal age. Our early methods were based on the fact that risk increases with age, and then on the idea that particular age cut-offs may signify varying levels of risk.
However, advances in ultrasound, and the identification of four pregnancy-related maternal blood analytes, provided us new and exciting insights on fetal status. These chemicals became part of a second-trimester screening process focused largely on trisomy 21. Although we still used age as a factor to assess risk, we learned that the cut-offs we had identified earlier were arbitrary and that risk could now be individualized.
 Photo courtesy Dr. Christopher Harman
Photo courtesy Dr. Christopher Harman
Figure 1. Two fetuses at 12 weeks' gestation, seen in profile. On the left, the narrow Nuchal Translucency (NT, the clear space behind the neck) and brightly echogenic nasal bone reduce the likelihood of aneuploidy. The fetus on the right has an NT over 4mm and nonvisualizing nasal bone. CVS on the second fetus revealed Down syndrome.
As research continued, it became apparent that versions of the biochemical tests used in second-trimester screening could be done in the first trimester – even by 12-14 weeks’ of gestation – and could be used to assess the risks not only of Down syndrome, but of other chromosomal abnormalities and some physical abnormalities. These biochemical tests (free beta-human chorionic gonadotropin and pregnancy-associated plasma protein-A) were combined with first-trimester ultrasound measurements of nuchal translucency into a screening algorithm that took hold more than 5 years ago and has steadily gained acceptance.
Since then, a number of parameters have been added to first-trimester screening to make the prediction of normality, or abnormality, even more precise. Assessment of the nasal bone, of the frontonasal facial angle, and of various structures inside the brain have become part of an anatomic review, for instance, that help us better define which babies we should be most concerned about.
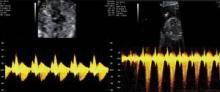 Photo courtesy Dr. Christopher Harman
Photo courtesy Dr. Christopher Harman
Figure 2. Another pair of fetuses appearing at 12 weeks for NT screening. Tricuspid valve Doppler shows normal flow on left. Fetus on right has large downward jet of Tricuspid regurgitation, suggesting possible abnormalities - pulmonary stenosis was later diagnosed.
Additionally, Doppler assessment of blood flow measurement – specifically of tricuspid regurgitation and of flow through the ductus venosus, a small fetal blood vessel that leads to the heart – can provide valuable information about fetal cardiac status and can easily be done in the context of the first-trimester ultrasound evaluation. Abnormal first-trimester Doppler findings also appear to predict Down syndrome and other adverse outcomes independently of a normal nuchal translucency measurement.
Combined with additional, early biochemical tests on maternal serum, these imaging advances (for fetal anatomic reviews and blood flow measurements) have led to an improved detection rate as high as 90% for trisomy 21 and other chromosomal abnormalities. More importantly, this detection rate is achieved without invasive testing, enabling us to reserve invasive procedures such as chorionic villus sampling (CVS) or amniocentesis for women with higher identified risks.
A New Cardiac Focus
The nuchal translucency test, which measures levels of fluid in a small area in the back of the fetal neck, has been available in the United States for approximately 15 years. With time, we have come to appreciate that a number of problems, in addition to Down syndrome, are associated with increases in nuchal translucency. We also better understand that abnormal nuchal translucency measurements are not always indicative of a problem, and that when there is a problem, the issue is not always chromosomal in nature.


