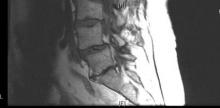
SNOWMASS, COLO. – The unremitting natural history typical of the syndrome of lumbar spinal stenosis makes surgery a particularly attractive therapeutic option for many patients with this common form of low back pain.
"Lumbar spinal stenosis patients, because of their age and comorbidities, face the highest risk from surgery, but they also have by far the most to gain because the natural history is so poor. So I spend a lot of time trying to get patients with low back pain due to a herniated disc to be patient, to use epidurals, to try a variety of different things to keep them out of the operating room. And I spend a lot of time helping the lumbar spinal stenosis patients overcome some of their fears and actually go ahead and elect surgery if they’re good candidates," Dr. Jeffrey N. Katz said at the symposium.
That being said, he added, there’s no rush. Rapid neurologic deterioration is rare in patients with lumbar spinal stenosis (LSS). Surgery usually can be deferred safely. About 20% of patients will experience symptomatic improvement over the course of a year, while a similar percentage will have symptomatic deterioration. The decision to undergo surgery should be based upon symptoms rather than on subtle neurologic deficits, which are highly unlikely to progress.
"Once people have well-established stenosis, things tend to sort of stay as they are," commented Dr. Katz, professor of medicine and orthopedic surgery Harvard Medical School, Boston, and professor of epidemiology and environmental health at the Harvard School of Public Health.
Surgery for LSS competes against a poor natural history, as compared with that of lumbago, in which 90% of episodes are resolved with conservative therapy within 3 months, or sciatica caused by a herniated disc, in which 90% of affected patients are improved with nonsurgical management by 6 months and 50% are asymptomatic at 1 year.
Findings from the multicenter SPORT (Spine Patient Outcomes Research Trial) study, the largest known randomized study of surgical vs. nonsurgical therapy for LSS, demonstrated an early and sustained outcome advantage favoring surgery through 2 years of follow-up (N. Engl. J. Med. 2008;358:794-810).
Unfortunately, the randomized portion of SPORT was rendered uninterpretable because of the extremely high treatment crossover rates in both the surgical and nonsurgical groups. Nevertheless, the as-treated analysis of 654 patients in the combined randomized and observational cohorts showed that the surgery group had a mean 19.8-point improvement in Short Form-36 bodily pain scores at 6 weeks and a 26.9-point gain at 2 years over a baseline of 31.4, which are effect sizes roughly twice those seen with conservative therapy, Dr. Katz noted.
Predictors of worsened functional status following surgery for LSS include worse preoperative self-rated overall health, back pain in excess of leg pain, less-severe radiographic stenosis, and a greater number of comorbid conditions.
The 1-year rate of reoperation for recurrent stenosis in SPORT was just 1.3%, compared with reoperation rates of around 10% in studies of discectomy for low back pain from a herniated disc. That high reoperation rate is the major shortcoming of discectomy, and it’s particularly problematic in view of the fact that reoperation has an even higher failure rate than first-time surgery.
Nevertheless, more than 400,000 discectomies are performed per year in the United States, a rate 1.5- to 5-fold higher than in other developed countries.
"I think the increased surgery rate in the U.S. has more to do with patient preferences than surgeon aggressiveness," he noted.
Patients who want to pursue nonsurgical therapy for LSS need to understand that it’s largely anecdotal in nature rather than evidence based. The most common elements include education regarding good posture, abdominal strengthening exercises, analgesics ranging from NSAIDs to narcotics, and epidural corticosteroid injections, which tend to provide more improvement in leg than back pain.
"A lumbar corset can be very helpful, because many of these people have an accompanying spondylolisthesis and symptomatic instability," Dr. Katz observed.
Aerobic exercise is highly beneficial as well.
"These people are much more comfortable in flexion than extension. It’s problematic for these patients to walk a lot, but they can very often bicycle ad lib. That’s a very useful thing to offer to patients," he said.
Dr. Katz wasn’t involved in the SPORT trial, which was supported by the National Institutes of Health and the Centers for Disease Control and Prevention. He reported having no financial conflicts with regard to his presentation.