Pregnant women who carry the hepatitis B e antigen are the subgroup of women at highest risk of transmitting hepatitis B virus (HBV) infection to their children who have been immunized, Dr. Huey-Ling Chen and her colleagues reported in the April issue of Gastroenterology.
The rate of "breakthrough" HBV infection was 9.26% among children of women who were positive for the hepatitis B e antigen, markedly higher than the 0.23% rate among children of women who were HBeAg negative.
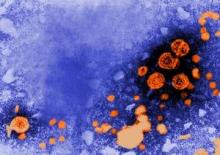 Photo courtesy CDC/ Dr. Erskine Palmert
Photo courtesy CDC/ Dr. Erskine Palmert
This transmission electron micrograph shows the presence of hepatitis B virions. In the Chen et al. study, the rate of breakthrough HBV infection was 9.26% in children born to HBeAg-positive mothers, compared with only 0.23% in children born to HBeAg-negative mothers.
Neonatal immunization does not eradicate mother-to-infant transmission of HBV completely, and the rate of breakthrough infection has been estimated to be at least 10%. Compared with individuals born in the preimmunization era, children who develop hepatitis B infection despite immunization are at higher risk of developing hepatocellular carcinoma, the investigators noted. "This population has been overlooked," they said.
Dr. Chen and her associates examined breakthrough HBV infection in what they described as the first large-scale study of children born to carrier mothers in Taiwan since universal neonatal HBV immunization was introduced there in 1984. Analyzing these data is crucial to "helping determine the government’s strategy for screening pregnant women, administering the neonatal HBV vaccine and the hepatitis B immunoglobulin program, and surveillance of high-risk children in the immunized population," they said (Gastroenterology 2012 April [doi:10.1053/j.gastro.2011.12.035]).
To do so, they performed a survey of 2,356 children born to mothers who carried the HBV surface antigen, a marker for HBV infection. The infants were delivered at nine tertiary referral hospitals across Taiwan during the period 1996 to 2008. A total of 583 of the children were born to HBeAg-positive mothers and 1,773 were born to HBeAg-negative mothers.
All of the children had documentation showing that they had received all three doses of the HBV vaccine as neonates. In addition, all the children of HBeAg-positive mothers had also received the mandatory hepatitis B immunoglobulin within 24 hours of birth. A total of 723 children of the HBeAg-negative mothers had received hepatitis B immunoglobulin at their parents’ request.
The rate of breakthrough HBV infection was 9.26% in children born to HBeAg-positive mothers, compared with only 0.23% in children born to HBeAg-negative mothers.
The overall rate of breakthrough infection, defined by positivity for antibodies against the hepatitis B core protein after 24 months of age, was 5.52%, but it also varied significantly based on the mothers’ hepatitis B e-antigen status. By this definition, the rate of breakthrough infection was 16.76% in children born to HBeAg-positive mothers, compared with 1.58% in children of HBeAg-negative mothers.
Similarly, the estimated rate of hepatitis chronicity was markedly higher in the children born to HBeAg-positive mothers (54%) than in those born to HBeAg-negative mothers (17%).
These differences are so large that "applying different preventive strategies to the two groups within a population-based program can be justified," said Dr. Chen, of the department of pediatrics at Taiwan University and the Hepatitis Research Center at National Taiwan University Hospital, both in Taipei, and her associates.
Now that children of e-antigen carriers have been identified as a subgroup that is particularly vulnerable to breakthrough hepatitis B infection, novel preventive methods should be targeted to these patients. For example, physicians might consider giving HBeAg-positive mothers antiviral therapy in late pregnancy to reduce the maternal viral load at delivery, the researchers said.
This vulnerable subgroup of children also would benefit from early and meticulous surveillance. "Despite breakthrough infection still occurring, HBV-related complications such as cirrhosis and hepatocellular carcinoma in the next generation may be minimized as much as possible through a well-conducted surveillance and secondary preventive system with good antiviral therapies," they noted.
In this study, it appeared that the use of hepatitis B immunoglobulin reduced the rate of breakthrough infection in children of mothers who were HBeAg negative. However, these data were misleading because the number of children who received the vaccine without immunoglobulin was quite low, and their infection rate was lower still.
"An extremely large sample size would be needed to test the difference in [breakthrough infection] rates between the two groups," and such a study does not appear feasible, Dr. Chen and her colleagues said.
This study was funded by the Center for Disease Control at the Taiwan Department of Health, and the National Taiwan University. No potential financial conflicts of interest were reported.

