BERLIN – Tocilizumab monotherapy worked substantially better than adalimumab monotherapy in a head-to-head randomized trial of 326 rheumatoid arthritis patients, suggesting that the newer drug tocilizumab has superior efficacy compared with drugs that block tumor necrosis factor, at least when methotrexate isn’t coadministered.
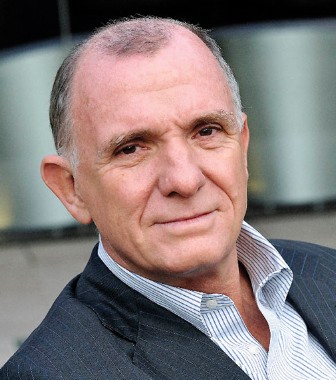
After 24 weeks of treatment, tocilizumab monotherapy produced remission of rheumatoid arthritis (RA) in 40% of patients, based on their disease activity score in 28 joints (DAS28), compared with an 11% remission rate in patients on adalimumab monotherapy, a significant difference, Dr. Cem Gabay reported at the annual European Congress of Rheumatology.
This is the first direct RA comparison of representatives of these two drug classes, both of which block cytokines, said Dr. Gabay, professor of pathology and immunology at the University of Geneva. Both tocilizumab (Actemra) and adalimumab (Humira) have Food and Drug Administration labeling for the treatment of RA.
"Anti-TNF [tumor necrosis factor] drugs remain the first biologic drugs to try, based on EULAR recommendations, but we showed that if a patient is on monotherapy, tocilizumab might be the better choice," Dr. Gabay said in an interview.
"If a patient is on methotrexate and tolerates methotrexate, there is no reason to stop," and those patients should continue to get a TNF inhibitor. "But many patients don’t tolerate methotrexate, and in these patients tocilizumab may be the choice for a biologic as monotherapy." About a third of RA patients who receive a biologic drug get it as monotherapy and are not on concomitant therapy with a synthetic, disease-modifying antirheumatic drug (DMARD) such as methotrexate, usually because they don’t tolerate those drugs or because their preference is to avoid them.
"This needs to be confirmed by other studies, but according to these new data, when patients cannot tolerate a synthetic DMARD they will do better on tocilizumab than with an anti-TNF drug," Dr. Gabay said. "But for the majority of patients [who are on synthetic DMARD treatment], an anti-TNF drug remains the first line. They have been around for 10 years, and are much more studied than tocilizumab."
The finding is important for RA practice because "we don’t have many head-to-head studies of biologics," commented Dr. Xavier Mariette, professor and head of rheumatology at Bicetre Hospital in Paris. But he questioned the fairness of using adalimumab as the study’s representative anti-TNF drug, noting its documented immunogenicity, especially when used in monotherapy. "Other monotherapy would have been more appropriate," he said.
In response, Dr. Gabay highlighted the separation in average DAS28 scores that occurred after 8 weeks of treatment between the two study arms, the point when patients on tocilizumab began to have significantly lower scores than the adalimumab patients. The difference seems to occur too soon to result from an immune reaction to adalimumab, Dr. Gabay said.
The ADACTA trial enrolled 326 adults with RA at 82 centers in 15 countries including the United States. Enrollment criteria included having RA for at least 6 months and a DAS28 score of more than 5.1. All patients were naive for biologic drugs, but they could have had prior or current treatment with methotrexate or other synthetic DMARDs. All DMARDs were withdrawn at least 2 weeks before the study began. The patients had a mean age of 53 years, 80% were women, their average RA duration was more than 6 years, they had a history with average of two DMARDs, slightly more than half were on an oral steroid, and their mean DAS28 score was about 6.7.
The researchers randomized patients to receive 8 mg/kg tocilizumab intravenously every 4 weeks, or 40 mg of subcutaneous adalimumab every 2 weeks. Patients also received placebo treatments to blind everyone to the active-drug assignments.
For the study’s primary end point, average change in DAS28 score from baseline to 24 weeks on treatment, the reductions averaged 1.8 points in the adalimumab group and 3.3 points in the tocilizumab group, a significant difference. Low disease activity, defined as a DAS28 score of 3.2 or less, occurred in 20% of the adalimumab patients and in 52% of those on tocilizumab, also a significant difference. A 20% improvement by the criteria of the American College of Rheumatology (ACR20) occurred in 49% of the adalimumab patients, and their ACR50 and ACR70 rates were 28% and 18%, respectively. In the tocilizumab patients, the ACR20/50/70 rates were 65%, 47%, and 33%, respectively.
The rates of serious adverse events, infections, and serious infections were all similar in the two treatment arms. Infections occurred in 42% of the adalimumab patients and in 48% of those on tocilizumab, and serious infections occurred in 3% of both groups. Serious adverse events occurred in 10% of the adalimumab patients and in 12% of those on tocilizumab. Patients on tocilizumab had moderately higher rates of elevated liver enzymes. The tocilizumab patients had a 31% rate of enzymes elevated from above the upper limit of normal (ULN) to 2.5-fold the ULN, compared with 25% of the adalimumab patients; and liver enzyme elevations of 2.6-5.0 times the ULN occurred in 6% of the tocilizumab patients and in 2% of those on adalimumab. Tocilizumab showed "no new or unexpected adverse effects," Dr. Gabay said.