Nearly 44% of multidrug-resistant tuberculosis cases tested in eight countries were also resistant to at least one second-line tuberculosis drug, according to results of an international prospective cohort study.
Extensively drug-resistant (XDR) strains were unexpectedly prevalent as well, particularly in South Korea and Russia, reported Tracy Dalton, Ph.D., of the Centers for Disease Control and Prevention, Atlanta, and colleagues. The report was published in the Aug. 30 online issue of The Lancet.
These XDR isolates were detected in 6.7% of patients overall, with prevalence in South Korea (15%) and Russia (11%) exceeding the current World Health Organization global estimate (9.4%). The risk of XDR disease was four times greater in previously treated patients, and previous treatment with second-line drugs was consistently the strongest risk factor for resistance to these drugs (Lancet 2012 Aug. 30 [http://dx.doi.org/10.1016/S0140-6736(12)60734-X]).
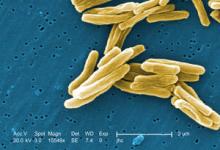
Multidrug-resistant (MDR) tuberculosis is resistant to at least rifampicin and isoniazid, and accounts for 3.6%-4.8% of new tuberculosis cases worldwide. XDR tuberculosis is resistant to at least rifampicin, isoniazid, and one or more of the second-line antituberculosis drugs. XDR tuberculosis has been reported in 77 countries.
While the numbers varied between nations, investigators with the international Preserving Effective TB Treatment Study (PETTS) saw a concerning pattern: The prevalence of drug-resistant strains correlated with the time that the second-line drugs had become available through the Green Light Committee, a World Health Organization program designed to increase access to second-line antituberculosis agents.
"[Second-line drugs] had been available for 10 years or less in Thailand (7 years), the Philippines (9 years), and Peru (10 years), and these countries had the lowest rates of resistance," wrote Dr. Dalton of the Centers for Disease Control and Prevention. "By contrast, South Korea and Russia had the longest histories of availability (more than 20 years) and the highest rates of resistance."
PETTS was launched in 2003 to determine the risk factors for and frequency of acquired resistance to second-line therapies in people with MDR tuberculosis. In 2005, in light of burgeoning numbers, the program was modified to include data on people with XDR tuberculosis.
The current report focused on eight countries: Estonia, Latvia, Peru, the Philippines, Russia, South Africa, South Korea, and Thailand. Samples from patients with MDR tuberculosis were obtained from large clinical centers in each country during 2005-2008. Inclusion criteria were at least 30 days of treatment with a second-line antituberculosis drug, with sputum collection within 30 days before or after the initiation of therapy.
Of 1,540 isolates tested, 1,278 (83%) were MDR. Most of those patients (94%) had a history of tuberculosis, and of those, 71% had experienced it at least once before the tested case.
Of the entire group, 93% had received first-line therapy, but only 15% had received second-line drugs. South Africa had the lowest rate of second-line treatment (3%), while South Korea had the highest (54%).
The overall prevalence of resistance to any second-line drug was 43.7%, but the rate varied among the countries, from 33% in Thailand to 62% in Latvia.
Overall, 20% of isolates were resistant to at least one second-line injectable drug, ranging from 2% in the Philippines to 47% in Latvia. The Philippines also had the lowest prevalence of resistance to all injectables (0.3%), while South Africa had the highest (26%).
The overall resistance rate to at least one second-line oral drug was 27%. Resistance to at least one oral drug ranged from 13% in Estonia to 38% in Latvia; however, other countries also had a high prevalence, including South Korea (36%), the Philippines (32%), Russia (26%), and South Africa (22%).
A total of 6.7% of the isolates were XDR, with the highest prevalence in South Korea (15%) and the lowest in the Philippines (0.8%).
Prior treatment for MDR strains with the second-line drugs was the strongest risk factor for XDR tuberculosis, with a relative risk of 4.75 for injectables and 4 for oral medications.
Although countries with Green Light projects did have more cases, the risks ratios for different resistance types did not reflect the actual numbers, the authors noted.
Resistance to fluoroquinolones and second-line injectable drugs – but not to other oral second-line drugs – was significantly less prevalent in countries that had Green Light Committee approved projects. "This difference was due to the very low prevalence of resistance to second-line drugs in the Philippines, which had the largest Green Light Committee project," the authors said.