Experts have coined a new term for the next phase of advancing in the quality of medical care: "systemness." You’ll be hearing more about systemness, to be sure.
Last week, the first national conference on creating systemness in health care delivery took place in Washington, convened by the ECRI Institute with help from large, successful medical systems including Kaiser Permanente; the Department of Veterans Affairs, and Sutter Health, to name a few.
So what is systemness? Here’s a graphic representation that conveys the complexity of what Dr. Kenneth W. Kizer calls "the new frontier of health care quality improvement."
If that’s not abstract enough for you, here’s the definition that Dr. Kizer provided at the first national symposium on quality cancer care held Dec. 1 by the American Society of Clinical Oncology: Systemness refers to the functional state of a collection of interconnected discrete parts that behave as a coherent whole in ways that are distinct from the component parts and that predictably and consistently produce results that are superior to the sum of the parts.
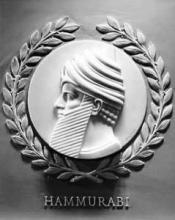
Even though the systemness conference and the quality cancer care conference were firsts, they’re part of at least a 4,000-year history of mankind’s quest to improve medical care. In a keynote address at the ASCO conference, Dr. Kizer picked a few highlights:
If a physician make a large incision with the operating knife and cure it ... he shall receive 10 shekels in money. If a physician make a large incision with the operating knife, and kill him ... his hands shall be cut off. – Code of Hammurabi, circa 1772 B.C.
Florence Nightingale, arguably the first modern health care improvement leader, set the foundation for the course that brought us to systemness today: "... even admitting to the full extent the great value of the hospital improvements in recent years, a vast deal of the suffering, and some at least of the mortality, in these establishments is avoidable."
In 1914, Dr. Ernest A. Codman advanced the idea of weeding out "bad apples" as part of quality control in medicine. By the middle of the 20th century, the health care industry started paying attention to what other industries were doing for quality improvements, including focuses on structure, process, and outcomes.
Only in the last 10-15 years have the science and technology of health care quality improvement matured enough to use these tools for advances, said Dr. Kizer, professor and director of the Institute for Population Health Improvement at the University of California, Davis.
The year 1998 was a tipping point, with major reports on the need to improve U.S. health care delivery published by the Institutes of Medicine, a presidential advisory commission, and the Milbank Quarterly, with other major reports on their heels. The quality of U.S. health care falls well below that achieved in other developed nations, and U.S. residents have a 50-50 chance, on average, of receiving recommended care, multiple studies reported.
Oh, and those other developed countries? They’ve got more systemness in health care than we do, apparently. In the United States, health care systems are highly heterogeneous, and many don’t yet show tangible synergies from systematizing, said Dr. Kizer.
As U.S. health care spending skyrockets, achieving systemness is essential for quality and sustainability, he said. It won’t happen on its own but must be intentionally designed and replicated. And because health care operates as a complex adaptive system, efforts to achieve systemness must be mindful of chaos theory – that unintended consequences are unavoidable and should be anticipated with vigilance built into the system.
The evidence for and understanding of systemness in health care is immature, but we know enough to conclude that there’s no single way to achieve it. Instead, 16 operating characteristic have been defined (so far), though most of the attention has fallen on infrastructure (IT, data sharing, etc.) and less on some of the "soft" components, Dr. Kizer said.
"Achieving systemness is about changing culture, fundamentally. It’s more about sociology than technology," and a culture of collaboration will develop in health care delivery only if financial incentives are aligned, he said. Accountable care organizations and bundled payments are mere steps along the way to greater systemness.
If all this is a bit too abstract for your taste, here’s a slightly more concrete and condensed summary: "Payment reform is inevitable," Dr. Kizer said. "Fee for service is dead."