Tedizolid, a second-generation oxazolidinone available in both oral and IV formulations, was found to be noninferior to linezolid for the treatment of acute, complicated infections of the skin and skin structure, including methicillin-resistant Staphylococcus aureus infections, according to a report in the Feb. 13 issue of JAMA.
In a phase III, randomized clinical trial, oral tedizolid phosphate (also known as TR-701) was at least as effective as oral linezolid early in the course of infection (at 48-72 hours after initiating therapy), and response to the drug persisted at a later follow-up at 7-14 days after treatment ended. Early effectiveness is important because clinicians decide whether to continue with their chosen agent or switch to different drugs during that period.
Tedizolid offers an advantage over linezolid in that it requires only once-daily dosing of a 200-mg tablet for a total of 6 days; the standard course of linezolid requires twice-daily dosing of a 600-mg tablet for 10 days. In this trial, tedizolid produced fewer gastrointestinal adverse effects and halved the rate of low platelet counts, compared with linezolid, said Dr. Philippe Prokocimer of Trius Therapeutics, San Diego, and his associates.
Trius, the maker of tedizolid, funded and conducted this 1-year, double-blind study at 54 medical centers in North America, Latin America, and Europe.
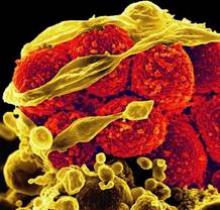
The researchers compared the two antibiotics in 667 adults (age range, 18-100 years) who had cellulitis/erysipelas, major cutaneous abscess, or wound infection surrounded by erythema, with a minimum total lesion surface of 75 cm2. The study subjects also had at least one local and one regional or one systemic sign of infection, and the infecting organism was either thought to be or proven to be a gram-positive pathogen.
The subjects were stratified by the presence or absence of fever at baseline, the geographic region where they resided, and the type of infection they had, and then randomly assigned to receive tedizolid (332 patients) or linezolid (335 patients). Both groups presented a similar clinical picture, with a median infected area of 188 cm; 87% of the study population had lymphadenopathy adjacent to the lesion, 41% had abnormal white blood cell counts, and 18% were febrile.
In the primary efficacy intention-to-treat analysis, 79.5% of the subjects receiving tedizolid and 79.4% receiving linezolid were classified as responders – meaning they were afebrile and their primary skin lesions had stopped spreading – when evaluated at 48-72 hours after the first dose of the antibiotics.
Conversely, 8.1% of the subjects receiving tedizolid and 10.4% of those receiving linezolid were true nonresponders, with fever or continued spread of the primary lesion, at 48-72 hours.
Thus, tedizolid met the criteria for noninferiority to linezolid at this time point, Dr. Prokocimer and his colleagues reported (JAMA 2013;309:559-69).
The remaining subjects were classified as "indeterminate" responders, usually because temperature data were missing or were only available outside the time window specified in the study protocol.
Secondary efficacy measures, sustained treatment response rates at two later follow-up times, followed a similar pattern. At the end of treatment, 69.3% of the tedizolid group and 71.9% of the linezolid group were deemed responders, and at final follow-up 1-2 weeks later, 80.2% and 81.1% were responders, respectively.
Results of several sensitivity and subgroup analyses confirmed those of these primary and secondary analyses. "Of particular interest are the similar treatment response rates in the tedizolid group (78%) and in the linezolid group (76.1%) in the sensitivity analysis that was based on the Foundation for the National Institutes of Health recommended outcome," which is a 20% or greater reduction in the lesion area.
Also of note was the finding that response rates were similarly high (approximately 85%) with both antibiotics in the subgroup of 178 patients who had methicillin-resistant Staphylococcus aureus (MRSA) infections.
Rates of adverse events and of serious adverse events were similar between the two study groups, with fewer patients in the tedizolid group reporting GI symptoms.
Postmarketing studies have reported possible links between linezolid and myelosuppression. in this study, low platelet counts were less than half as frequent in the subjects who received tedizolid as in those who received linezolid, but the analysis "was not adequately powered to make conclusions about the risk of myelosuppression with tedizolid," the authors said.
The investigators reported ties to Trius, Cerexa, Achaogen, and other companies.