HONOLULU – The answers to six questions can identify 18% of the stroke-free general population as having a greater than 40% chance of hospitalization or an emergency department visit for cardiovascular disease within the next 5 years, according to a large national study.
New evidence from the REGARDS (Reasons for Geographic and Racial Differences in Stroke) study indicates that the predictive power of the six questions compares to that of traditional cardiovascular risk factors, Virginia J. Howard, Ph.D., said at the International Stroke Conference sponsored by the American Heart Association.
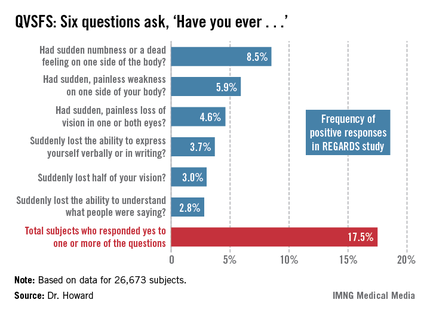
These six questions – called the Questionnaire for Verifying Stroke-Free Status, or QVSFS – can easily be asked by office staff during a routine patient evaluation. Although the questions relate to strokelike symptoms, they also were predictive of other cardiovascular events.
REGARDS is a prospective, population-based, longitudinal study of 30,239 African Americans and whites over age 45. The national study oversampled African Americans, who made up 40% of the study population.
Dr. Howard’s analysis was restricted to the 26,673 subjects, mean age 64 years, with no baseline history of stroke or transient ischemic attack (TIA). Of these participants, 49% characterized their general health as excellent or very good, and another 35% described it as good. Yet 57% of subjects had hypertension, 32% were dyslipidemic, and 21% had diabetes.
During a mean 5.6 years of follow-up, 30% of subjects were hospitalized or had an emergency department visit for heart disease, stroke (9%), or TIA.
Fully 17.5% of subjects answered one or more of the questions affirmatively at baseline (see chart). Their rate of hospitalization or an ED visit for cardiovascular disease during the follow-up period was nearly twice that of patients who answered ‘no’ to all six questions.
In a multivariate analysis fully adjusted for demographics, socioeconomic status, conventional cardiovascular risk factors, and self-reported general health, subjects with any positive answer on the QVSFS at baseline had a 62% greater incidence of hospitalization or an ED visit for cardiovascular disease and a 47% greater incidence of hospitalization or a trip to the ED for stroke than did those who answered ‘no’ to all six questions, reported Dr. Howard of the University of Alabama, Birmingham.
A positive response to a single QVSFS question was provided by 10.5% of subjects. Another 4.6% gave affirmative answers to two questions, 1.4% did so for three, and 0.9% gave four or more positive answers.
In the fully adjusted multivariate analysis, each additional positive response was associated with an additional 29% increase in the risk of a cardiovascular hospitalization or ED visit and a 22% increase in the risk of a hospitalization or ED visit for stroke.
Looking at traditional cardiovascular risk factors, subjects with hypertension had a 12% greater risk of cardiovascular hospitalization or an ED visit and a 17% greater risk of stroke hospitalization or an ED visit. Diabetes conveyed a 29% greater risk of cardiovascular hospitalization or an ED visit and a 43% increase in stroke risk.
The REGARDS study is funded by the National Institute of Neurological Disorders and Stroke. Dr. Howard reported having no financial conflicts.