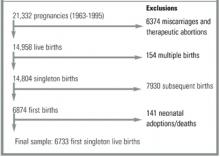
FIGURE
Study sample
Variable definitions
Pregnancies were categorized as either intended or unintended at conception, using new definitions established by the Institute of Medicine in 1995.3 Pregnancies were considered intended if a woman had stopped using birth control because she wanted to become pregnant. Unintended pregnancies were classified into 1 of 2 categories: (1) mis-timed: wanted pregnancies that occurred sooner than desired, or (2) unwanted: pregnancies that occurred while a woman was using contraception and had not ever wanted to have a(nother) baby. The 170 women who described their pregnancy intention status as “didn’t know” or “didn’t care” were excluded from analyses involving intention status as defined above. There were 2 breastfeeding outcomes in this study: (1) initiation of breastfeeding, including women who reported any breastfeeding at all, and (2) duration of non-exclusive breastfeeding for at least 16 weeks.
Maternal demographics, intrapartum and postpartum behaviors, and birth outcomes were considered as potential confounders. As missing data were imputed in the public use data file, information on each variable was complete, except where noted below. Maternal age was determined at the time of conception. Education was defined as completed years of schooling at the time of the interview. Race was categorized as white, black, Hispanic, or other. Marital status was defined as either married or not married. Socioeconomic status was measured continuously as a percentage of the 1995 poverty level. Information on prenatal care was only available for births in the last 5 years (n=1266). For the 1241 women who reported that they had received prenatal care, the mean weeks of gestation at the time of the first prenatal visit were calculated. Maternity leave was defined as the use of maternity leave, paid or unpaid, for women who were working during the pregnancy (n=3662). For those who took any leave, the mean length of that leave was calculated in weeks. The 33 women for whom data were not available and the 5 women who answered that they took 0 weeks of maternity leave were not included in this calculation. Infant variables were considered categorically: mode of delivery, either vaginal or cesarean; prematurity, birth at less than or equal to 36 weeks; and low birth weight, less than or equal to 5.5 pounds.
Statistical analysis
The statistical significance of descriptive variables was determined using 2-sample t tests and chi-square tests, with women who did not breastfeed at all as the comparison group.
To compare our results with existing literature, we calculated crude odds ratios of not breastfeeding and used chi-square tests to assess the statistical significance of these associations. The reference group was always women whose pregnancies were intended. Variables identified as potential confounders were age, race, marital status, poverty level, education, maternity leave, mode of delivery, prematurity, and low birth weight. Final logistic regression models were adjusted for those variables that changed crude odds ratios by 10% or more: age, race, marital status, poverty level, and education. Adjusted odds ratios (ORs) of not breastfeeding and 95% confidence intervals (CIs) are reported.
Effect modification was assessed by dichotomizing each of the 5 confounding variables in the following manner: teen versus 20 years or older; white versus black versus Hispanic (here, the 193 women in the sample who defined their race as other were not included); married versus unmarried; high school education or higher versus less than a high school education; and below the poverty level versus at or above the poverty level. Each stratified analysis was adjusted for the other 4 factors. Interaction terms were created and P values for heterogeneity were calculated for all logistic models. For race, an additional interaction term was created to compare white with non-white (black and Hispanic combined) women.
These data are contained on the National Survey of Family Growth Cycle 5 1995 CD-ROM, Series 23, No. 3 and were exported using SETS version 1.22a (National Center for Health Statistics, Hyattsville, MD). All analyses were performed with SAS version 6.12 (SAS Institute, Cary, NC). Odds ratios are weighted using sampling weights provided in the data set. SUDAAN version 7.5.3 was used to obtain standard errors (Research Triangle Institute, Research Triangle Park, NC).
Results
In the total sample of 6733 first singleton live births to US mothers, 3267 (48.5%) of women initiated breastfeeding, compared with 3466 (51.5%) who did not. In the entire sample, 1775 (26.4%) continued to breastfeed nonexclusively for at least 16 weeks.
The breastfeeding initiation rate was 55.9%, 37.4%, and 28.0% for women with intended, mis-timed, and unwanted pregnancies, respectively. By 16 weeks, 32.6%, 17.0%, and 15.5% of women, respectively, were still breastfeeding. For all women who breastfed, the mean number of weeks of breastfeeding was 24.4 (standard deviation = 24.9; range = < 1 week to 4.0 years). Only 3.9% of women who breastfed did so for more than 2 years.